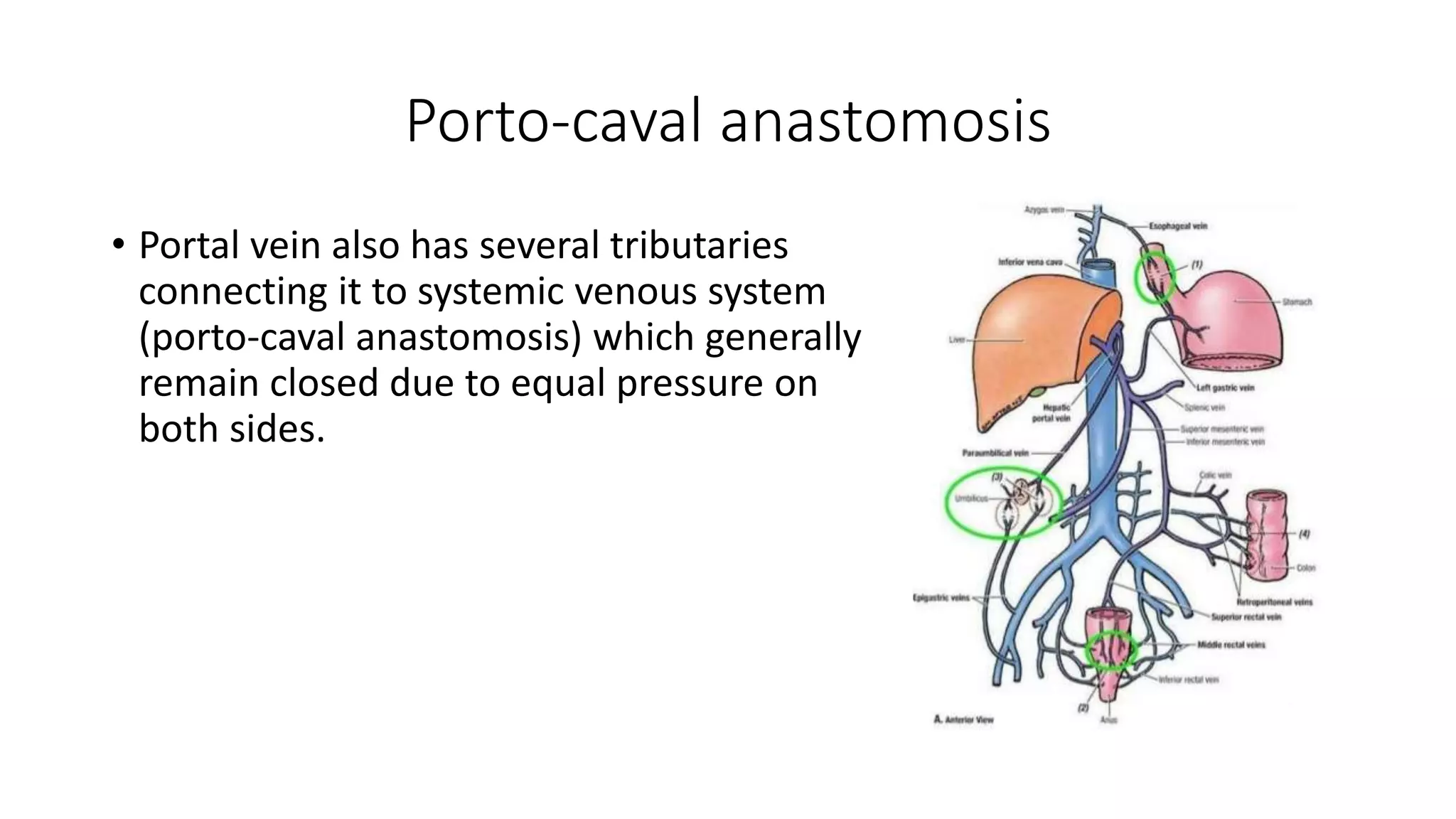
The portal vein is formed by the superior mesenteric and splenic veins. It drains blood from the intestines, pancreas, colon and rectum. Blood from the portal and hepatic arteries mixes in the liver sinusoids before draining into the hepatic vein and inferior vena cava. Portal hypertension occurs when pressure increases due to increased resistance in the liver from cirrhosis and increased blood flow. It can cause ascites, variceal bleeding, and other complications.