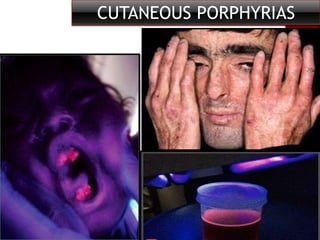
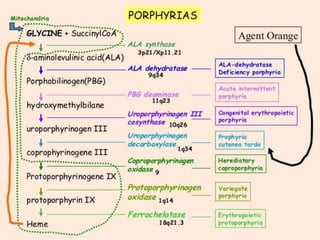
This document discusses various types of cutaneous porphyrias (porphyrias that affect the skin):
1. Porphyria cutanea tarda is the most common type, caused by a deficiency in the enzyme uroporphyrinogen decarboxylase. It causes fragile blistering skin in sun-exposed areas and is associated with liver disease.
2. Congenital erythropoietic porphyria is a very rare, severe disorder causing lifelong photosensitivity and scarring. It is caused by a deficiency in uroporphyrinogen cosynthase, leading to accumulation of porphyrins in red blood cells.
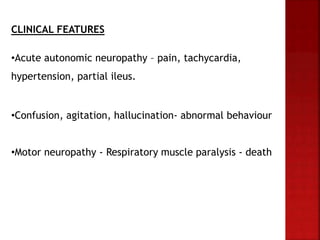
3. Acute