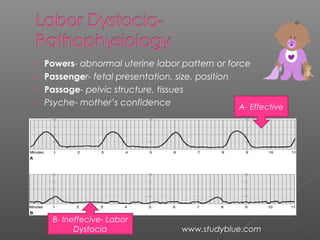
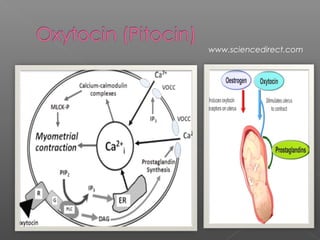
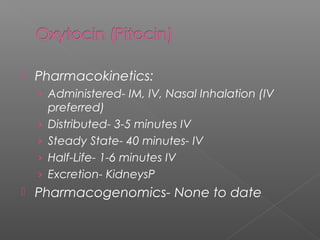
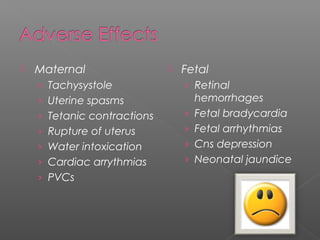
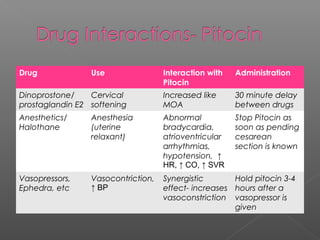
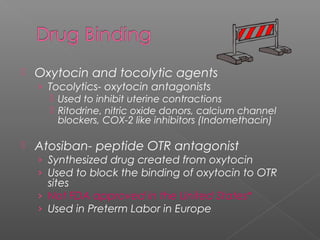
Oxytocin is the most common drug used to induce and augment labor. Its use has increased significantly since the 1990s. Oxytocin works by binding to oxytocin receptors in the uterus and increasing intracellular calcium and prostaglandin levels, resulting in uterine contractions. While it effectively stimulates labor when used properly, it also carries maternal and fetal risks if overused or improperly administered, such as tachysystole and fetal distress. Hospitals have implemented safety protocols like double nurse checks for high risk medications like oxytocin to help mitigate risks.