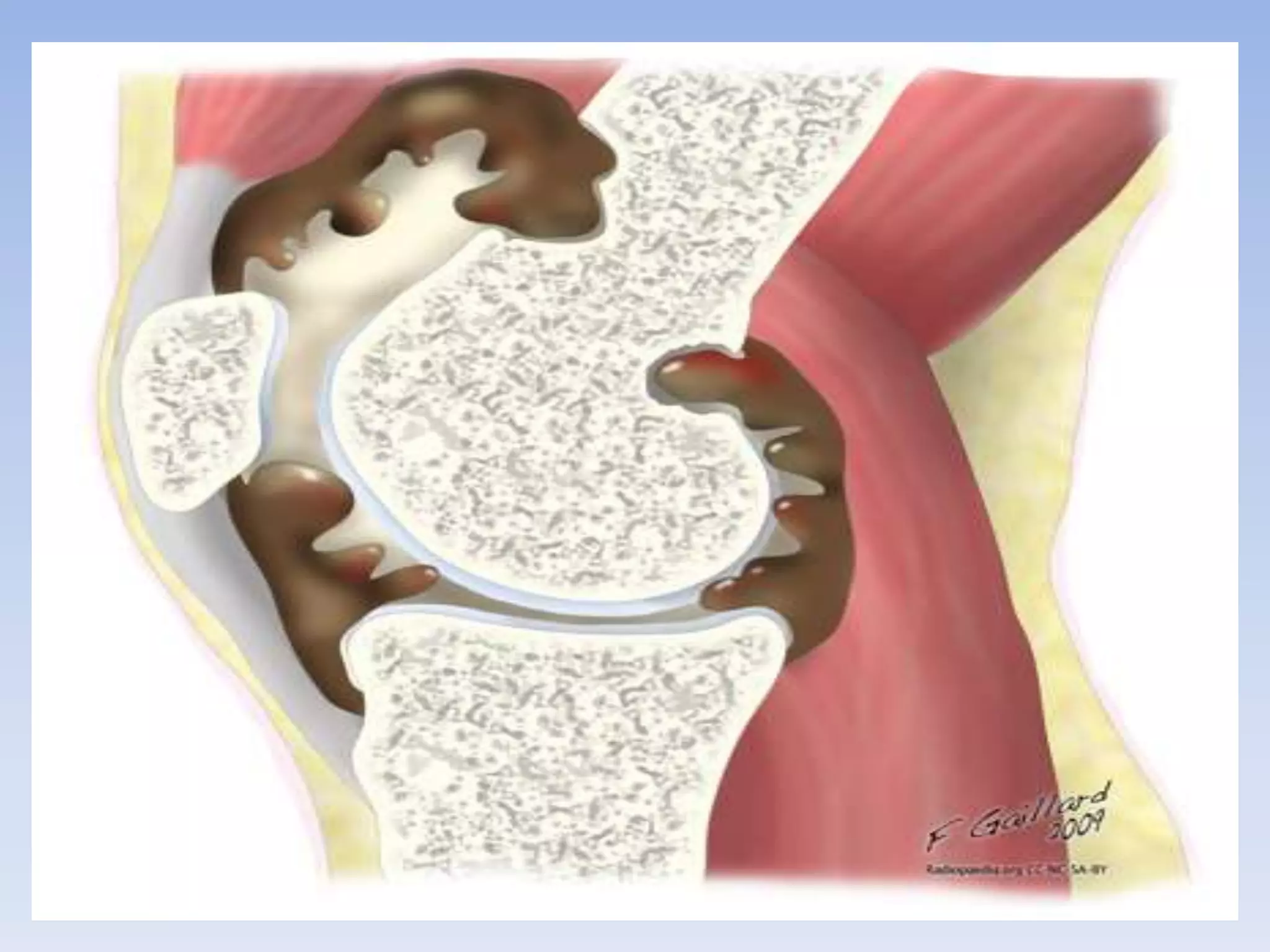
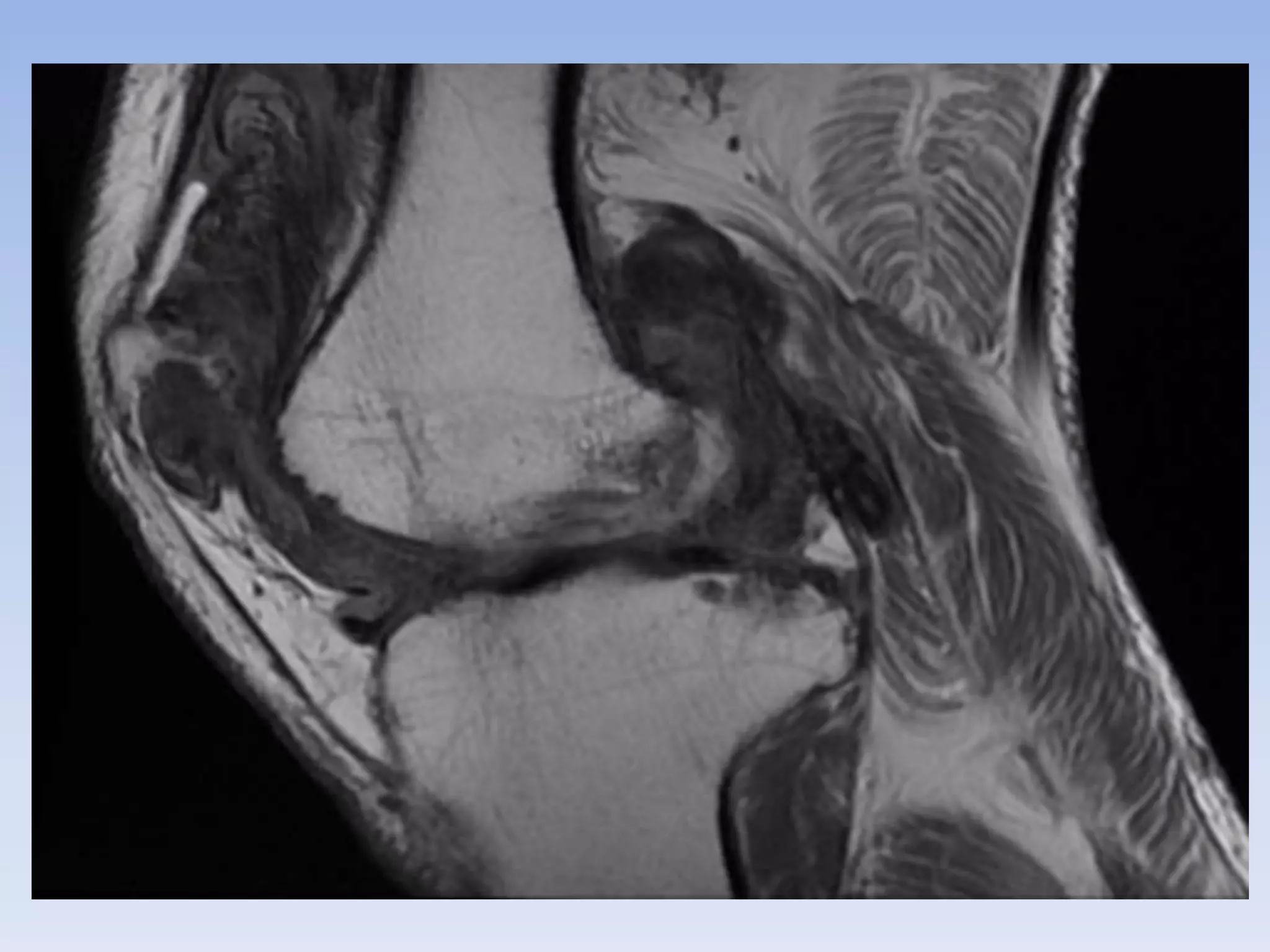
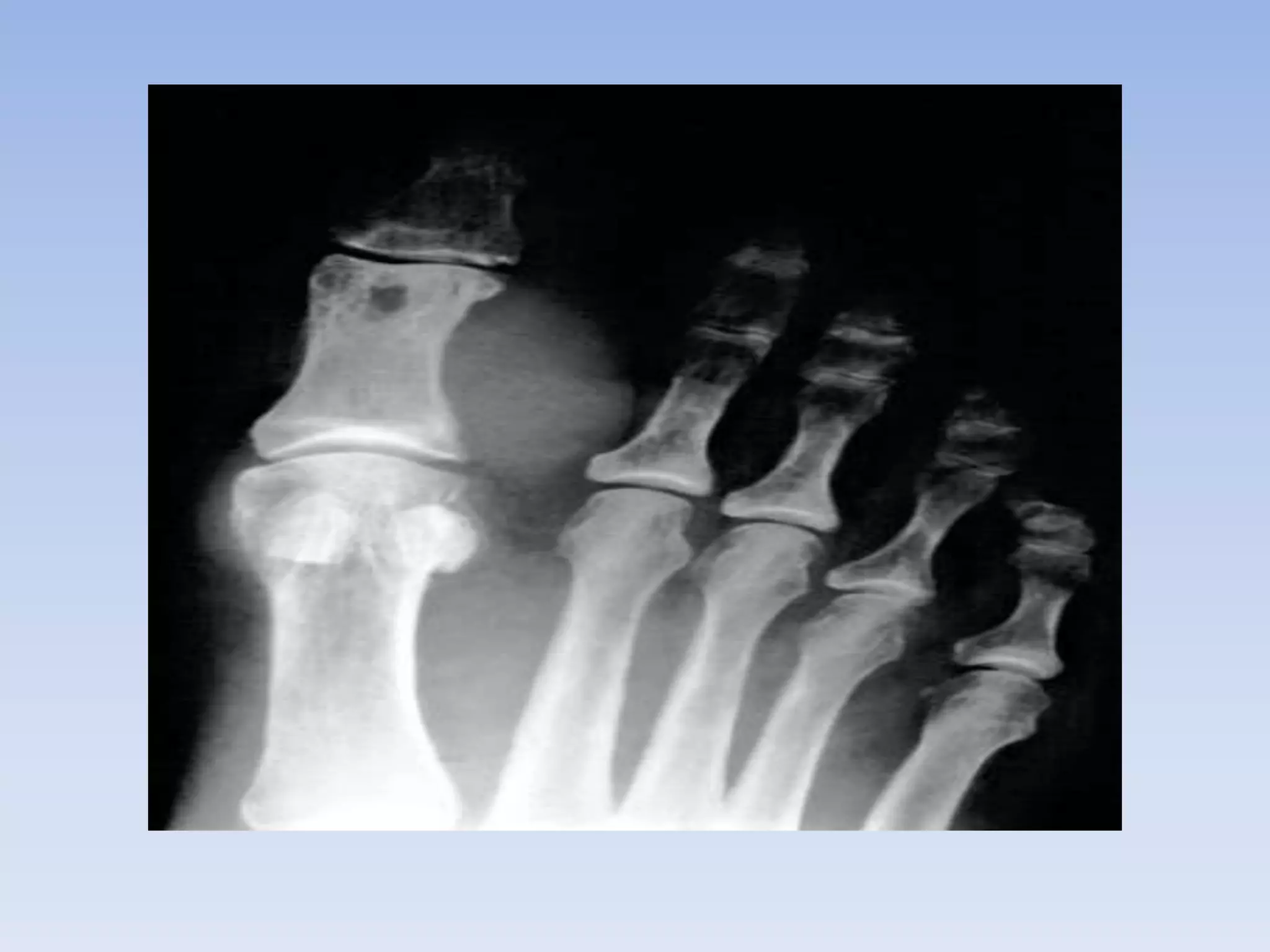
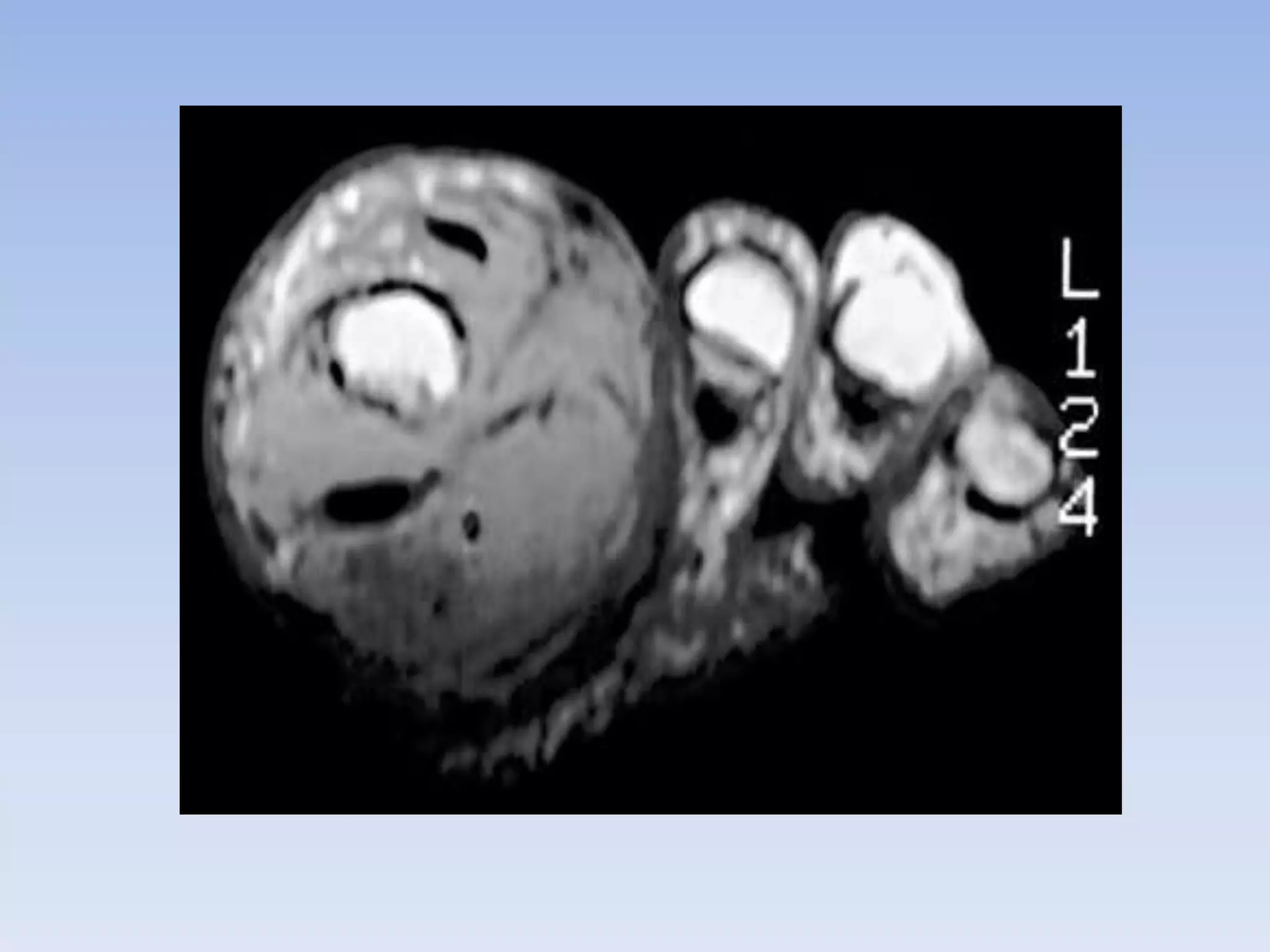
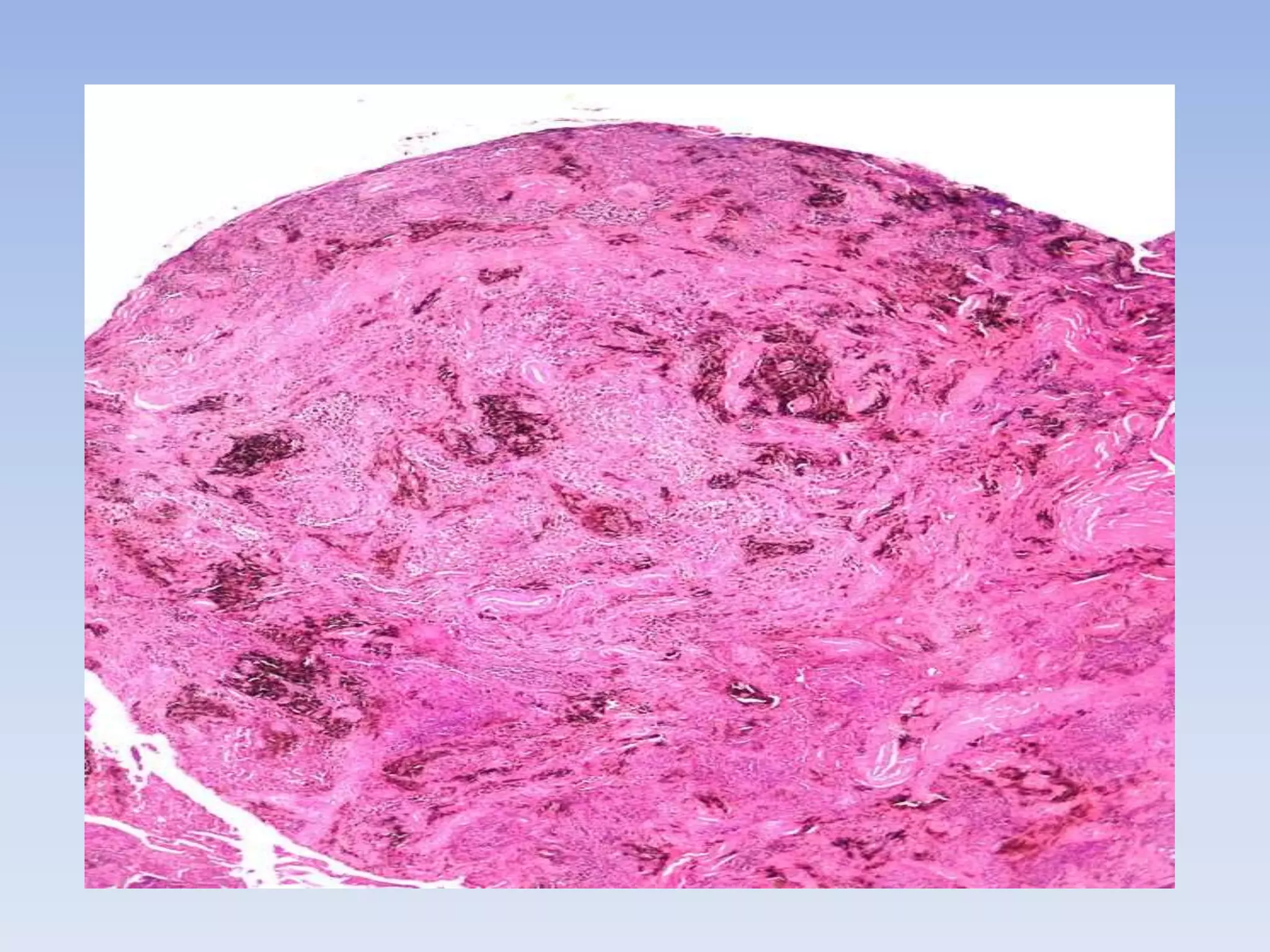
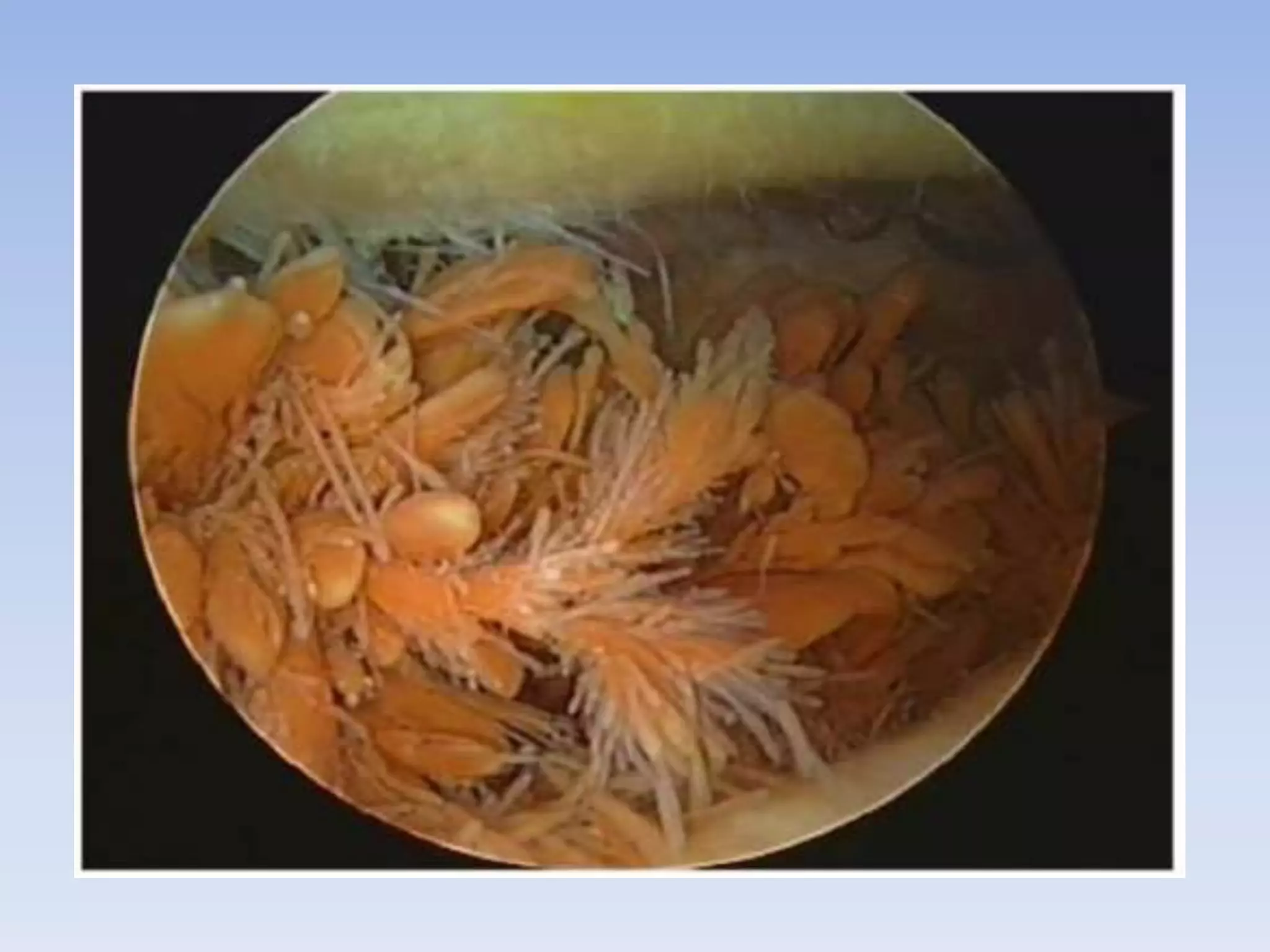
Pigmented villonodular synovitis (PVNS) is a benign proliferative disorder of unknown cause that affects synovial joints, bursae, and tendon sheaths. It is characterized by inflammation and overgrowth of the joint lining. There are two primary forms - a diffuse form affecting the entire synovial lining and a rare localized form occurring in small joints. While the cause is unknown, it is thought to be neoplastic in nature. Treatment involves complete surgical resection or radiation therapy to prevent recurrence, as incomplete removal can allow regrowth. Radiation therapy provides effective local control with minimal side effects.