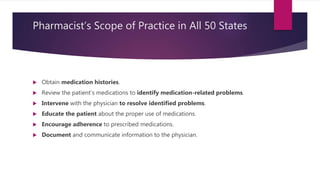
This document outlines the scope of practice for pharmacists and models of pharmacy care. It discusses that pharmacists' scope is regulated at the state level and includes interpreting, evaluating, dispensing, and implementing medical orders as well as providing patient care services. Two common models of pharmacy care discussed are pharmaceutical care, which involves optimizing patient health outcomes, and medication therapy management, which ensures best therapeutic outcomes for patients through medication therapy reviews and follow-up.