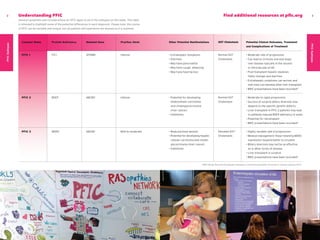
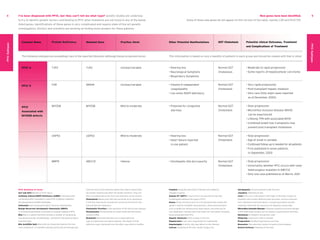
This document provides information about Progressive Familial Intrahepatic Cholestasis (PFIC), a rare genetic liver disease. It defines what PFIC is, describes potential symptoms, diagnostic testing and treatment options. It also outlines the three main subtypes of PFIC, defined by the gene that is mutated. Each subtype can present with different levels of itching and liver abnormalities, and may progress to complications like liver failure if left untreated. Close monitoring by medical experts and potential surgical interventions or liver transplant are important for managing PFIC.