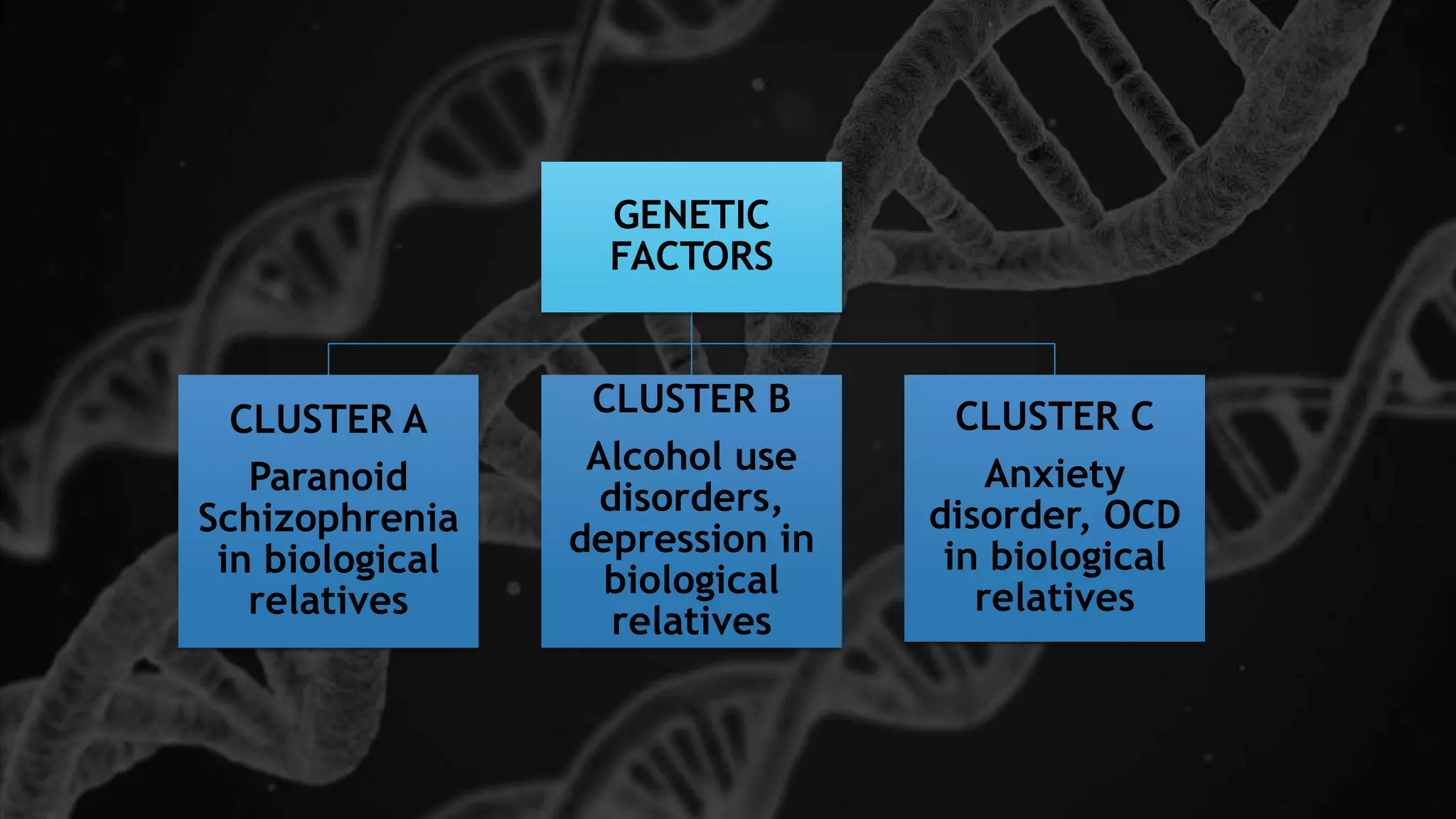
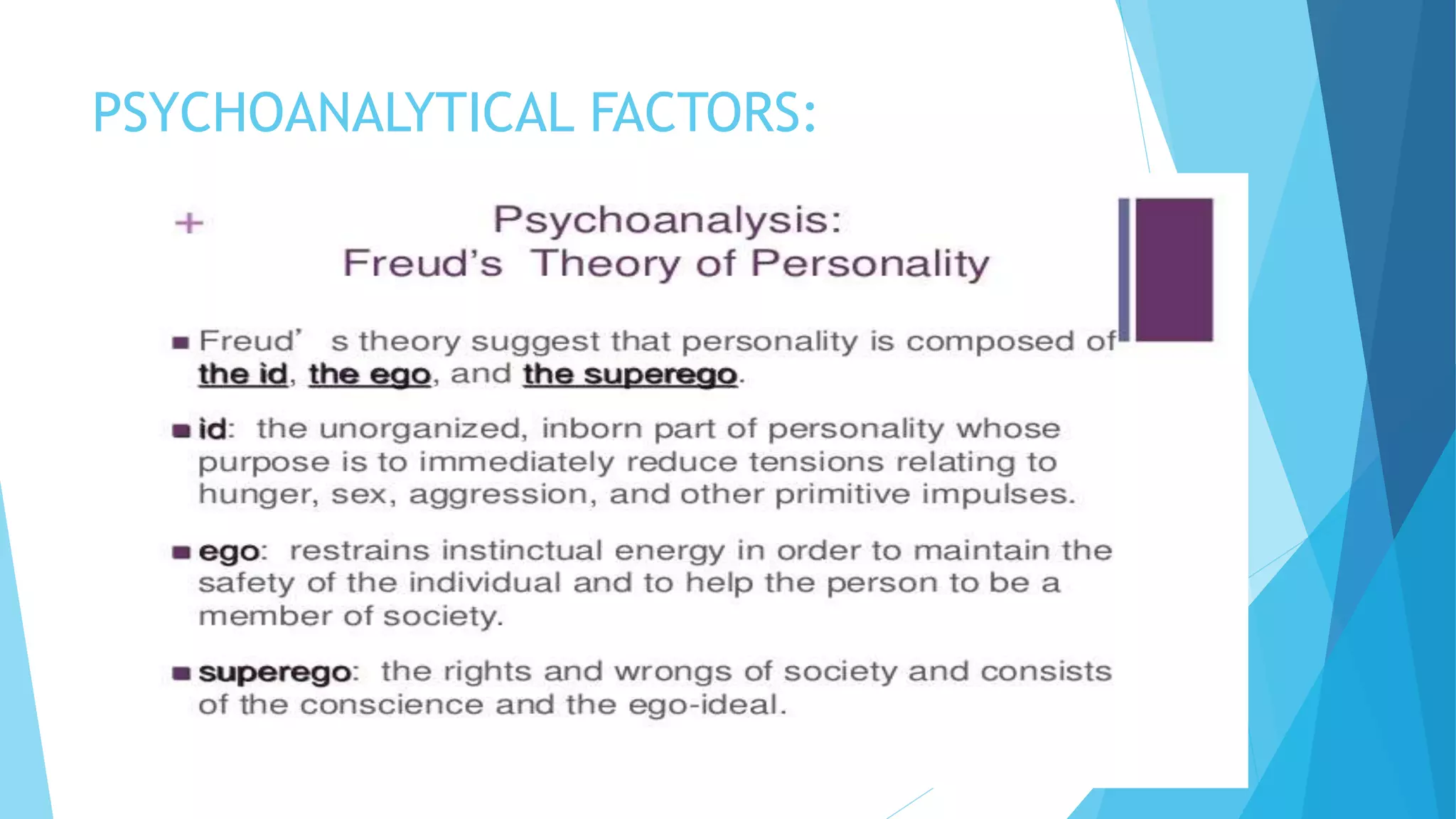
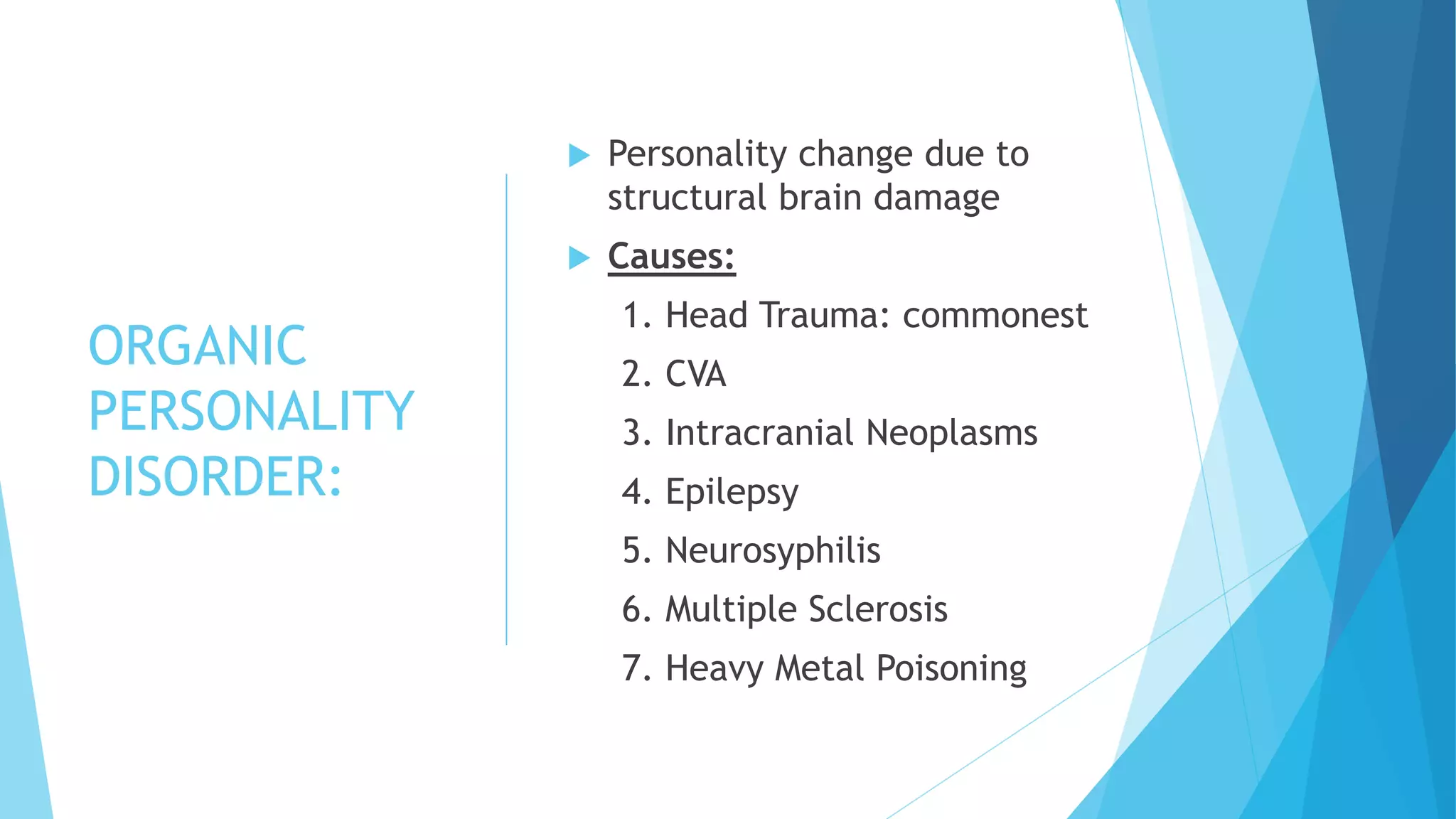
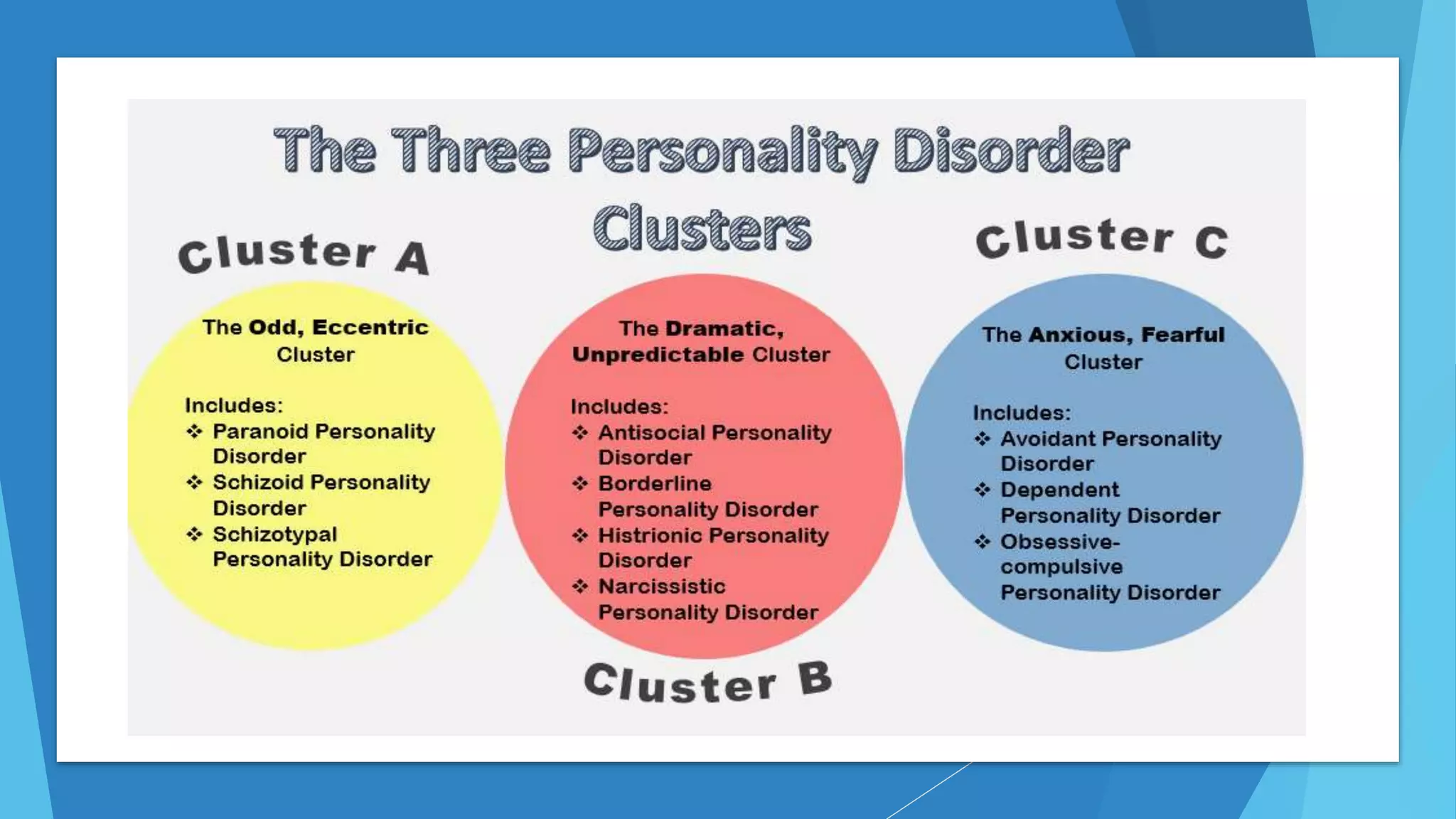
This document provides information on personality disorders including definitions, characteristics, prevalence, etiology, and treatment. It defines personality and personality disorders. Personality disorders are diagnosed when personality traits become inflexible and maladaptive. Common personality disorders discussed include paranoid, schizotypal, schizoid, antisocial, borderline, histrionic, narcissistic, avoidant, dependent, and obsessive-compulsive personality disorders. Etiology may include genetic and biological factors as well as psychoanalytical factors. Treatment involves pharmacotherapy such as antidepressants, antipsychotics, and mood stabilizers as well as psychotherapy including CBT and DBT. Examples of characters from television exhibiting personality disorders are also provided.




















![PHARMACOTHERAPY:
1. ANTI- DEPRESSANT
SSRI: Mostly in depressive symptoms
associated with BPD, ASPD, Avoidant,
Dependent & OCPD.
OCPD: High dose of SSRI [Fluoxetine,
Fluvoxamine, Sertraline, Escitalopram]
TCA: Clomipramine, adjunctive therapy in
OCPD
Imipramine: In Nocturnal enuresis,
common in BPD
NDRI: Bupropion, in smoking cessation in
BPD, ASPD, decreases performance anxiety in
cluster C
MAOI: Decreases aggression in Schizotypal,
ASPD](https://image.slidesharecdn.com/personalitydisorders-200731195447/75/Personality-disorders-32-2048.jpg)




![PHEOBE [FRIENDS]
SCHIZOTYPAL
HEAD BUTLER
[REMAINS OF THE
DAY]
SCHIZOID
JERRY
[CONSPIRACY
THEORY]
PARANOID](https://image.slidesharecdn.com/personalitydisorders-200731195447/75/Personality-disorders-40-2048.jpg)
![Dr. HANNIBAL LECTER
[HANNIBAL] ASPD
RON [ANCHORMAN]
NARCISSISTIC
SUSANNA [GIRL,
INTERRUPTED] BPD
SCARLETT [GONE WITH
THE WIND]
HISTRIONIC](https://image.slidesharecdn.com/personalitydisorders-200731195447/75/Personality-disorders-41-2048.jpg)
![SHELDON COOPER [BIG BANG THEORY]
OCPD
ROSS [FRIENDS] DEPENDENT](https://image.slidesharecdn.com/personalitydisorders-200731195447/75/Personality-disorders-42-2048.jpg)
