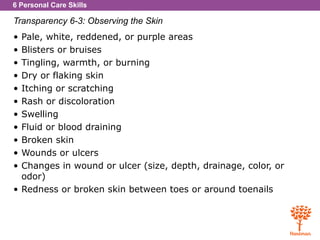
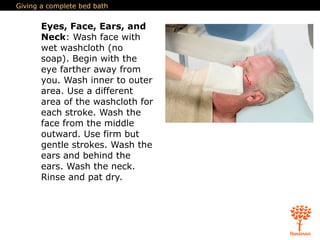
The document provides guidelines for NAs in assisting with personal care of residents, including bathing and skin care. It defines key terms and outlines best practices for NAs to follow when providing personal care. Specifically, it describes how to properly assist with a bed bath, including washing each body part in a respectful manner that maintains privacy and promotes the resident's dignity, independence, and skin health. NAs are instructed to observe the resident's skin and report any changes to the nurse.