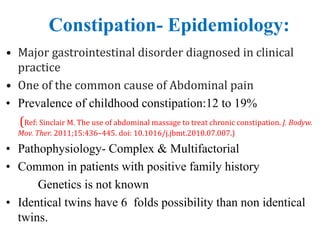
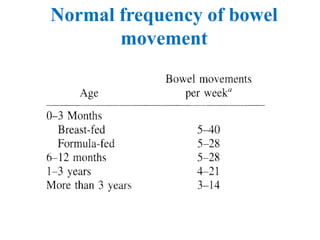
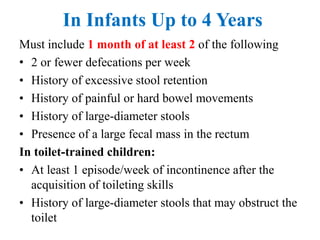
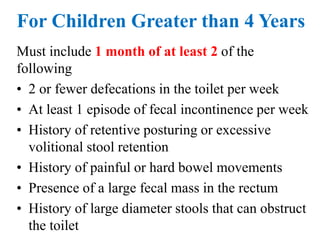
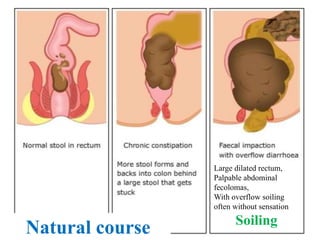
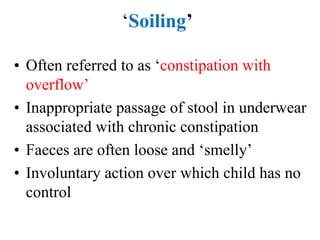
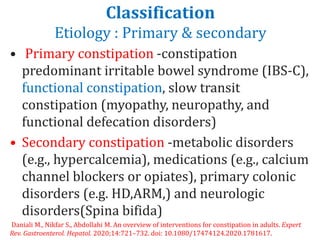
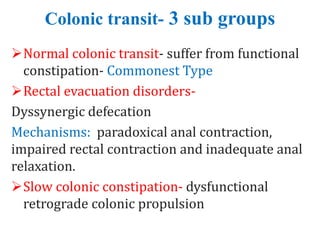
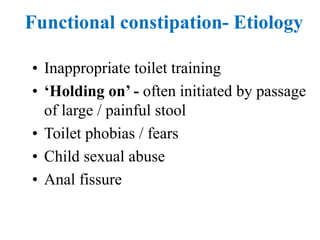
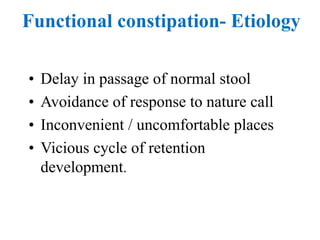
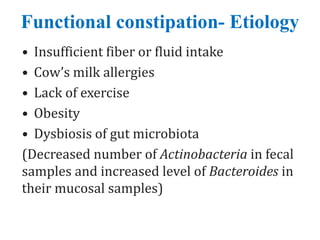
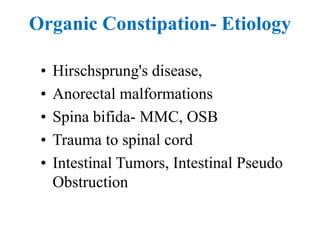
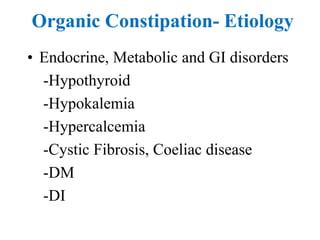
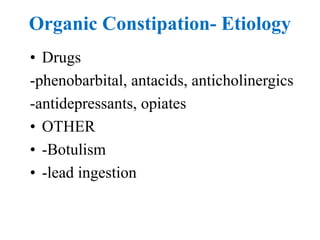
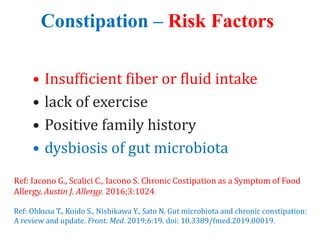
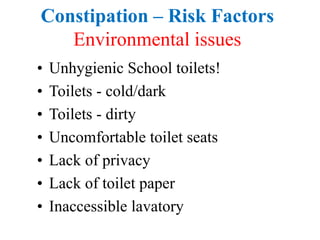
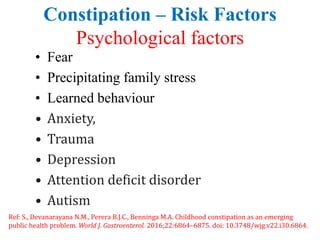
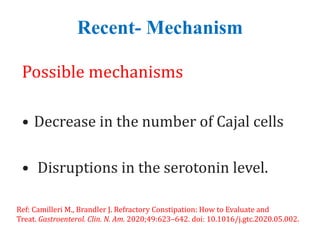
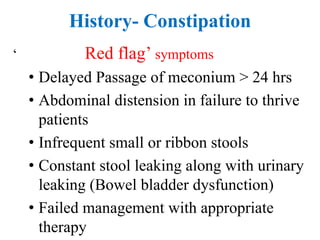
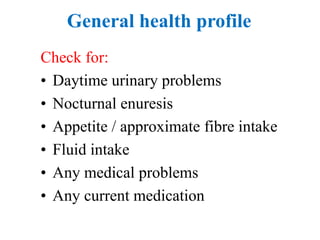
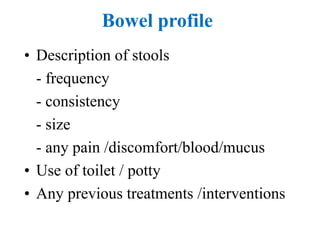
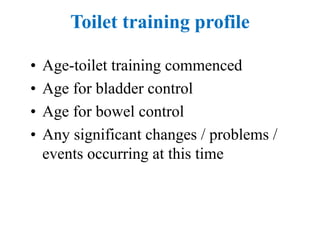
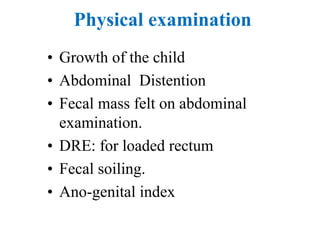
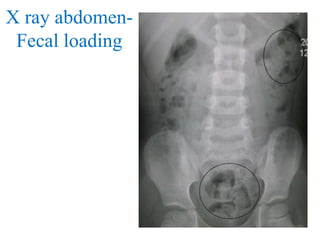
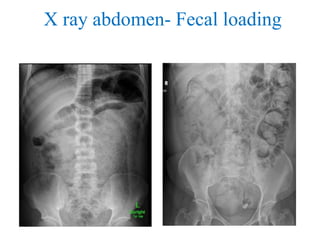
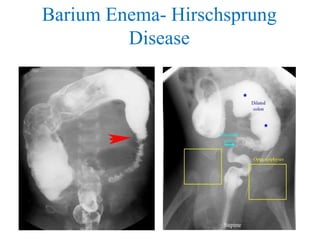
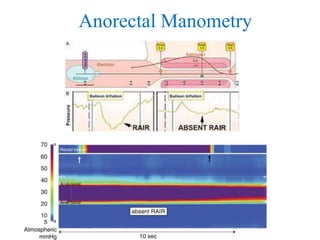
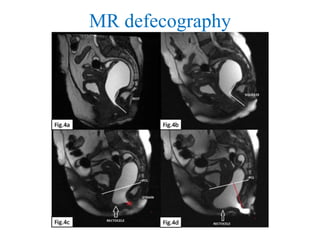
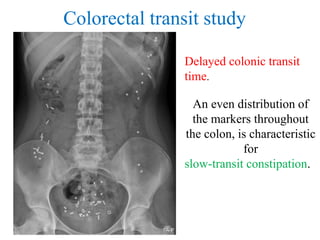
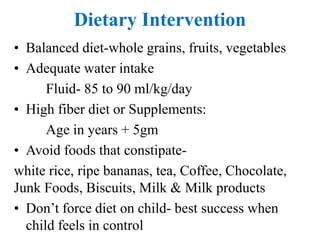
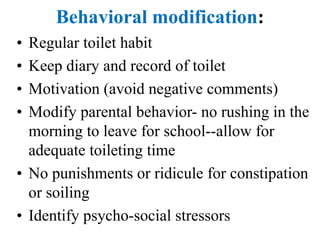
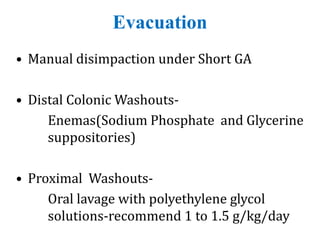
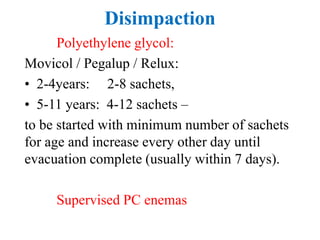
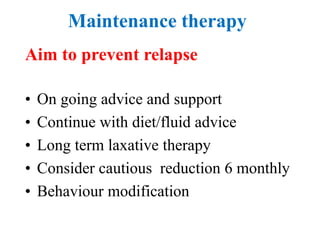
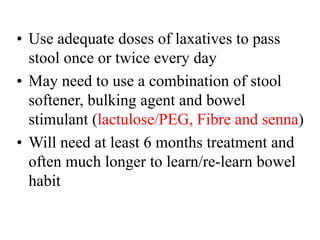
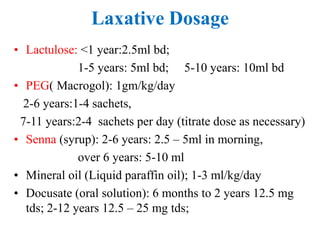
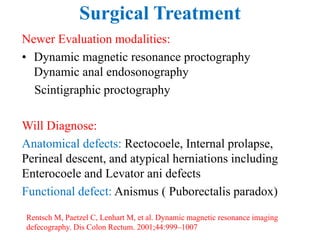
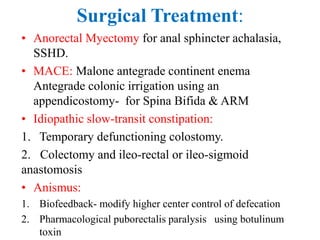
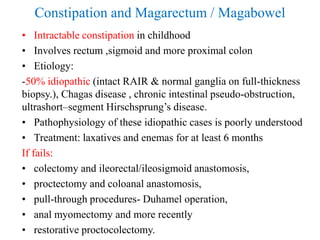
Constipation is a common gastrointestinal issue in children. It can be functional or organic in nature, with functional constipation making up the majority of cases. The document discusses the definition, epidemiology, risk factors, evaluation, and management of pediatric constipation. Evaluation involves history, physical exam, and potential imaging and testing. Management is multi-pronged, focusing on education, dietary changes, behavioral modifications, disimpaction if needed, and long-term maintenance therapy often involving laxatives. Surgery is rarely needed and reserved for severe, refractory cases. Childhood constipation can sometimes predict irritable bowel syndrome in adulthood.