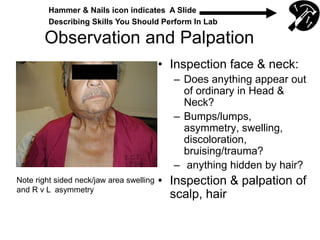
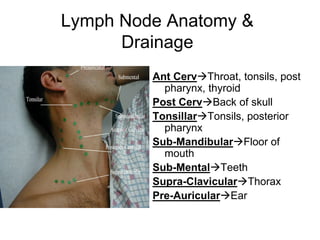
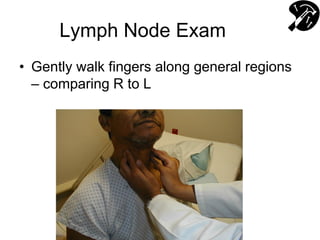
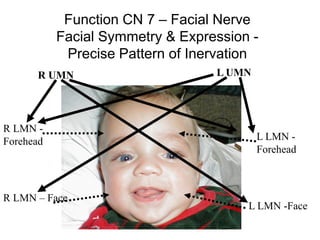
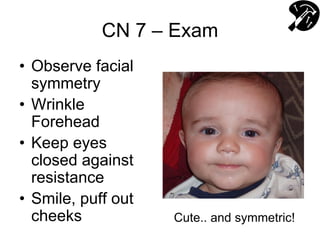
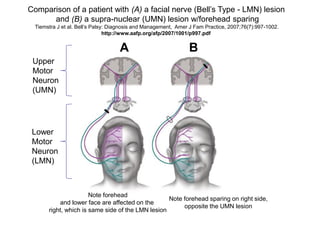
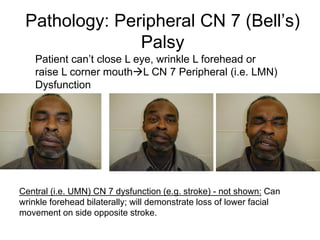
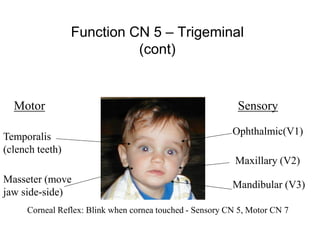
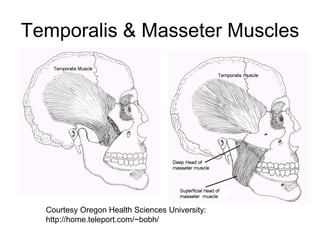
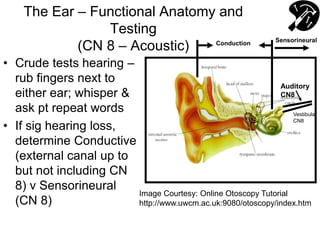
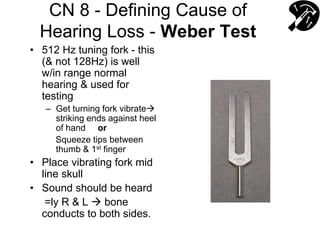
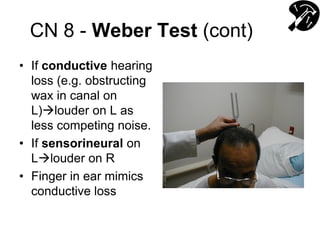
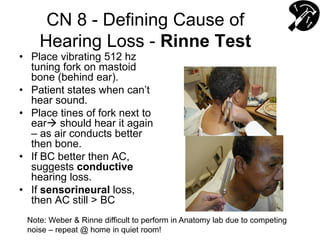
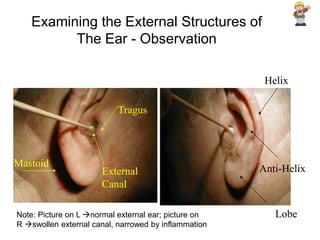
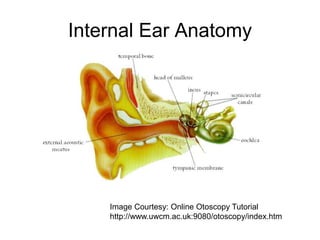
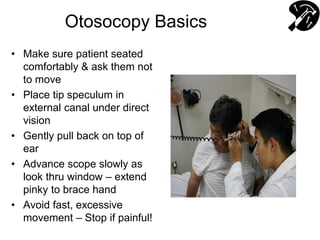
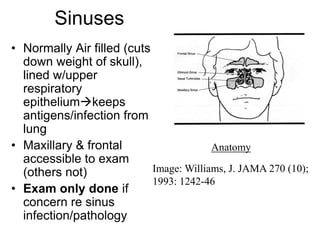
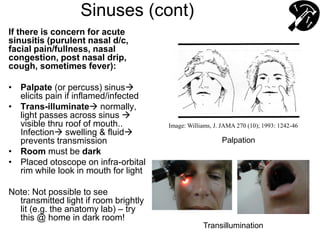
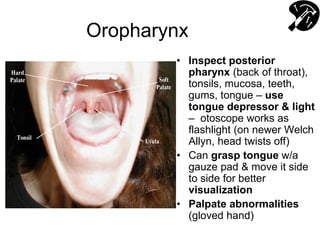
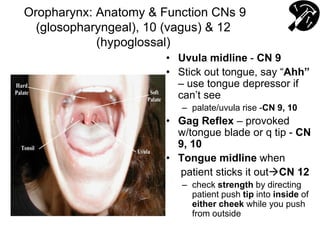
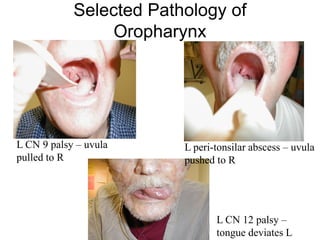
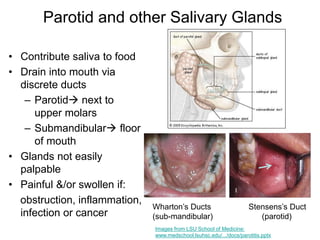
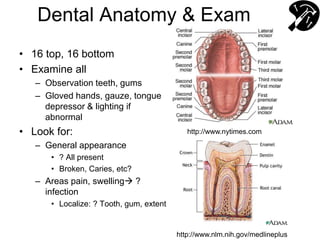
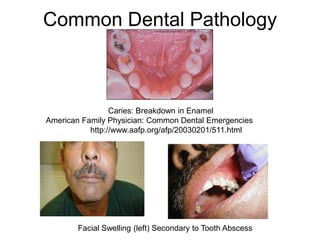
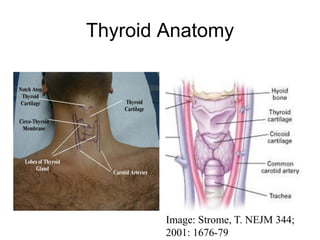
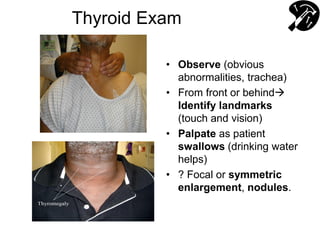
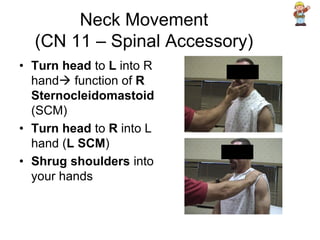
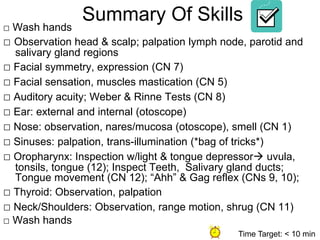
This document provides guidance on performing a head and neck exam. It describes how to inspect the face, neck, scalp, and hair for abnormalities. It also details how to palpate lymph nodes in the head and neck region. The document reviews anatomy of the lymph nodes and their drainage patterns. It provides information on evaluating cranial nerves 5, 7, and 8 by testing sensation, movement, and hearing. Examination of the nose, sinuses, mouth, throat, salivary glands, teeth, and thyroid is also outlined.