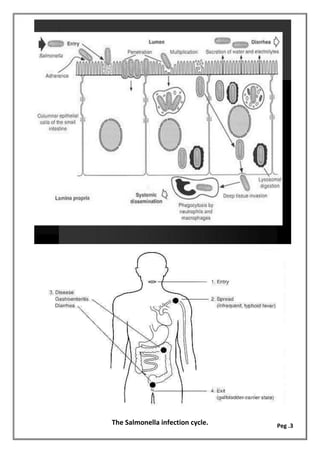
The document provides an overview of various pathogenic bacteria, their characteristics, and the diseases they cause, particularly focusing on Salmonella and Shigella species. It discusses their mechanisms of pathogenicity, laboratory diagnosis, and treatment options for infections such as salmonellosis and shigellosis. Additionally, it includes information on other bacteria such as Klebsiella, Mycoplasma, and Vibrio cholerae, along with their clinical significance and diagnostic methods.