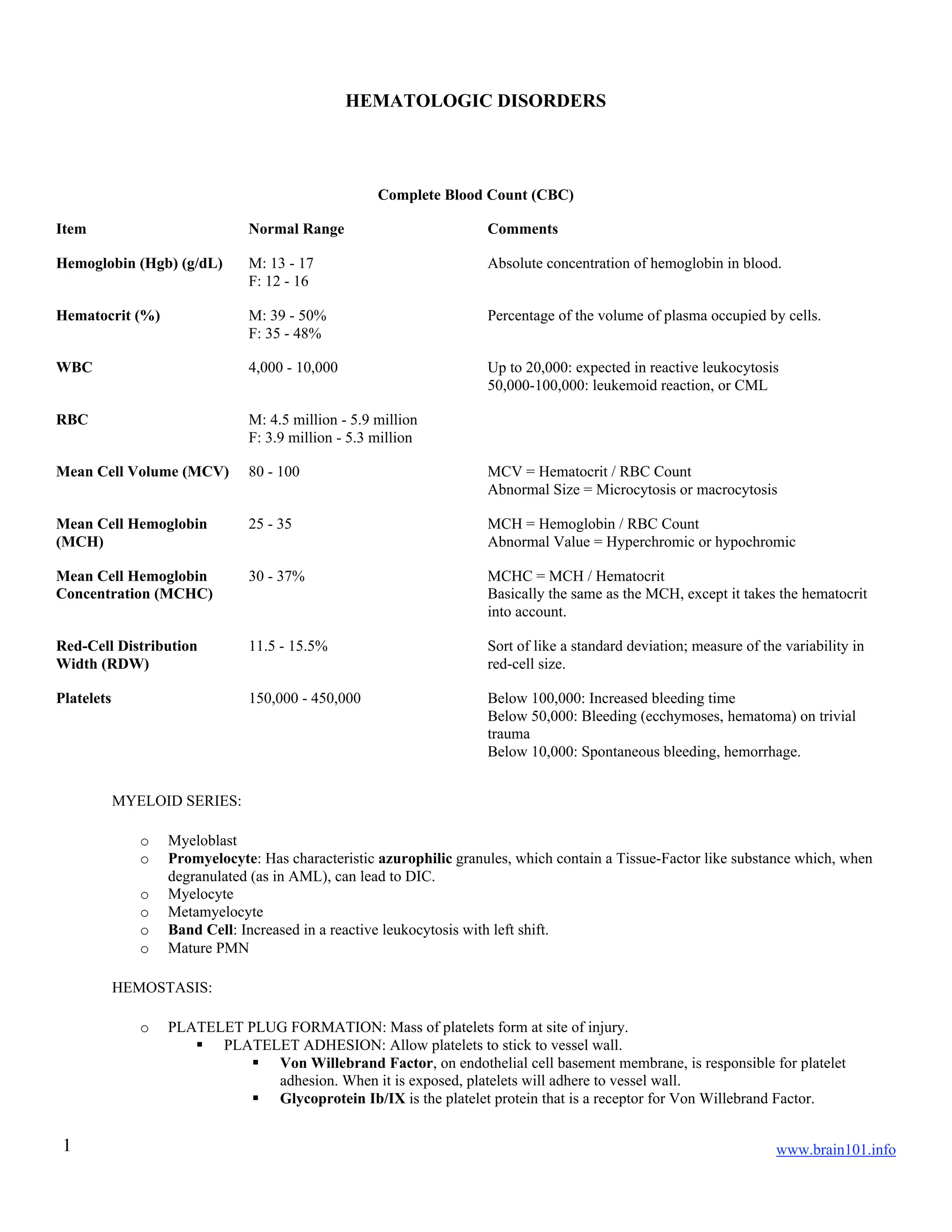
This document provides information on hematologic disorders and complete blood count (CBC) parameters. It discusses normal ranges for components like hemoglobin, hematocrit, white blood cell count, red blood cell count, and platelet count. Mean cell volume, hemoglobin, and hemoglobin concentration are also explained. Various blood disorders are summarized, including anemias, bleeding disorders, and abnormalities in coagulation and platelet function.