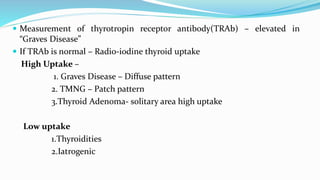
This document discusses hypothyroidism and hyperthyroidism. It defines primary and secondary hypothyroidism, and lists common causes such as iodine deficiency, autoimmune diseases, drugs, and radiation therapy. Signs and symptoms of hypothyroidism are described. Diagnosis involves measuring TSH and free T4 levels. Treatment is typically levothyroxine, with monitoring of medication levels and watch for complications like myxedema coma. Hyperthyroidism is also outlined, with causes like Graves' disease, toxic multinodular goiter, and excess iodine intake. Diagnosis and treatment approaches are summarized.