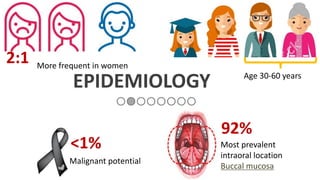
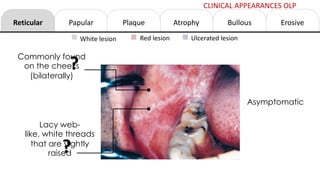
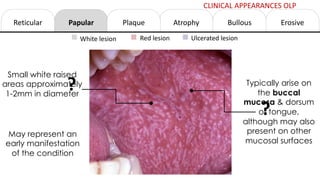
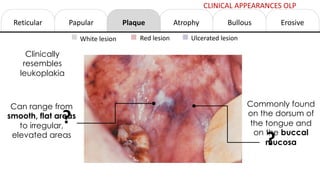
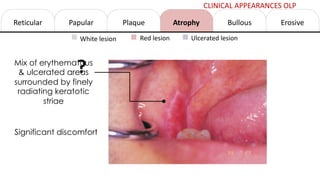
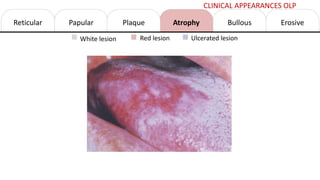
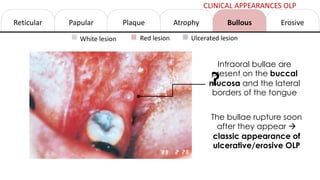
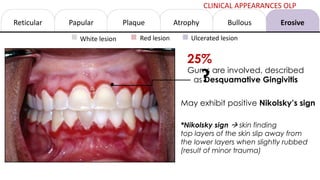
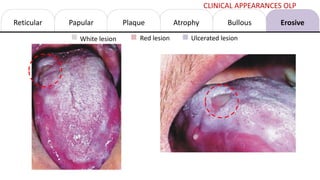
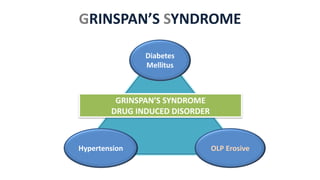
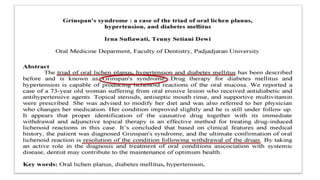
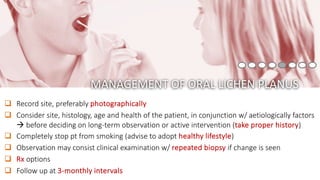
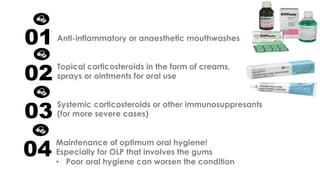
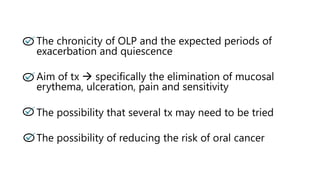
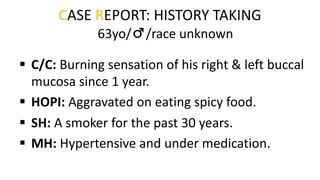
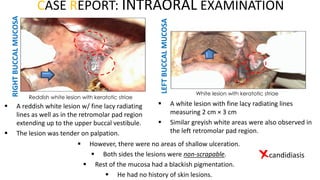
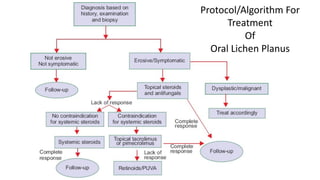
This document provides information on oral lichen planus (OLP), including its definition, epidemiology, etiology, clinical presentations, management, and treatment. OLP is a common chronic inflammatory mucocutaneous disorder that typically affects the oral mucosa. Clinically, it presents as reticular, papular, plaque-like, atrophic, or erosive lesions. Management involves observation, stopping smoking, topical corticosteroids, immunosuppressants, and maintaining good oral hygiene. While there is no cure for OLP, treatment aims to reduce symptoms and potentially lower cancer risk.









![• Zain RB, Ikeda N, Reichart P, Axell T. 2002.Clinical Criteria for Diagnosis of Oral Mucosal Lesions: An Aid for Dental and Medical
Practitioners in the Asia-Pacific Region. Faculty of Dentistry, University of Malaya. Kuala Lumpur
• Scully, C. (2008). Oral and maxillofacial medicine- The basis of diagnosis and treatment. (2nd ed.) Elsevier.
• Eisen D, Carrozzo M, Bagan Sebastian JV, Thongprasom K: Number V Oral lichen planus: Clinical features and management. Oral
Dis 2005; 11:338-349.
• van der Meij EH, Schepman KP, van der Waal I: The possible premalignant character of oral lichen planus and oral lichenoid lesions: A
prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96:164-171.
• Bornstein MM, Kalas L, Lemp S, et al: Oral lichen planus and malignant transformation: A retrospective follow-up study of clinical and
histopathologic data. Quintessence Int 2006; 37:261-271.
• Roosaar A, Yin L, Sandborgh-Englund G, et al: On the natural course of oral lichen lesions in a Swedish population-based sample. Oral
Pathol Med 2006; 35:257-261.
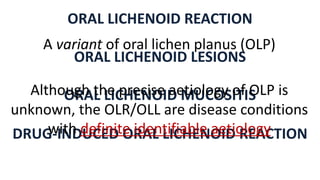
• Al-Hashimi I, Schifter M, Lochart PB, et al: Oral lichen planus and oral lichenoid lesions: Diagnostic and therapeutic considerations. Oral
Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103(Suppl S25):e1-e12.
• 573. Porter SR, Kirby A, Olsen I, Barrett W: Immunologic aspects of dermal and oral lichen planus. Oral Surg Oral Med Oral
Pathol 1997; 83:358-366.
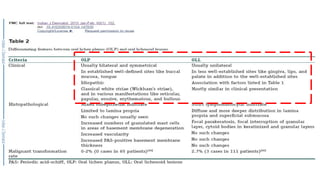
• Do Prado RF, Marocchio LS, Felipini RC. Oral lichen planus versus oral lichenoid reaction: Difficulties in the diagnosis. Indian J Dent Res
[serial online] 2009 [cited 2016 Oct 11];20:361-4. Available from: http://www.ijdr.in/text.asp?2009/20/3/361/57375
• Kamath VV, Setlur K, Yerlagudda K. Oral Lichenoid Lesions - A Review and Update. Indian Journal of Dermatology. 2015;60(1):102.
doi:10.4103/0019-5154.147830.
REFERENCES](https://image.slidesharecdn.com/orallichenplanus-231114070931-5fa16948/85/Oral-Lichen-Planus-34-320.jpg)
