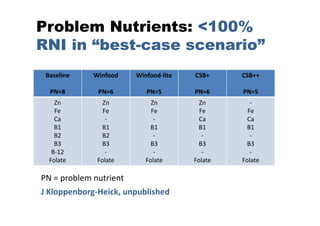
The document introduces 'Optifood', a linear programming tool designed to enhance nutrition program planning and policy decisions in Southeast Asia, addressing under-nutrition. It outlines how Optifood can formulate food-based recommendations, assess nutrient adequacy, and analyze food affordability and availability to ensure dietary sufficiency for specific target groups. The tool aims to provide evidence for effective interventions and advocacy concerning nutritional needs in various populations.