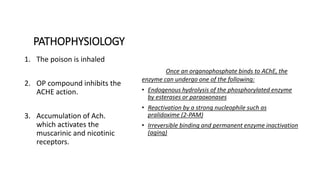
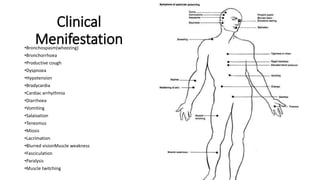
Organophosphate poisoning occurs when someone is exposed to organophosphate compounds, which are commonly found in insecticides, nerve agents, and other chemicals. These compounds work by inhibiting acetylcholinesterase, leading to excess acetylcholine in the body and stimulation of muscarinic and nicotinic receptors. Symptoms include bronchospasm, vomiting, diarrhea, muscle weakness and paralysis. Diagnosis is made through history, physical exam, checking acetylcholinesterase levels in blood and urine. Treatment involves atropine to counteract excess acetylcholine, pralidoxime to reactivate acetylcholinesterase, benzodiazepines for seizures, and supportive care. Prognosis depends on
![INTRODUCTION
Organophosphate (OP) compounds
are a diverse group of chemicals
used in both domestic and
industrial settings. Examples of
organophosphates include
insecticides (malathion, parathion,
diazinon, fenthion, dichlorvos,
chlorpyrifos, ethion), nerve gases
(soman, tabun, VX), ophthalmic
agents (echothiophate,
isoflurophate), and antihelmintics
(trichlorfon). Herbicides (tribufos
[DEF], merphos) are tricresyl
phosphate–containing industrial
chemicals.](https://image.slidesharecdn.com/op-170306071813/85/Oppoisoning-2-320.jpg)