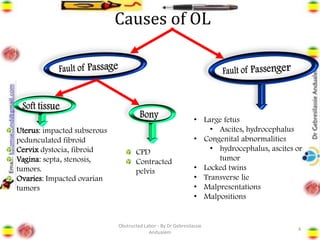
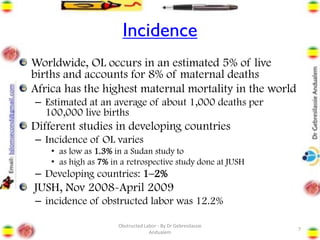
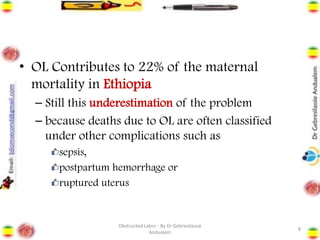
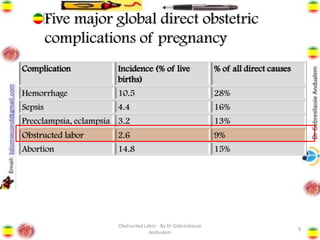
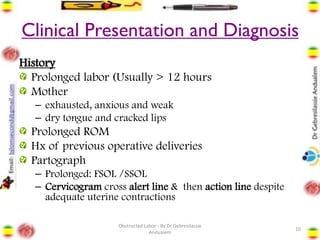
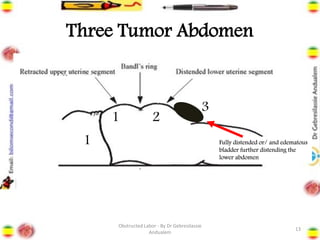
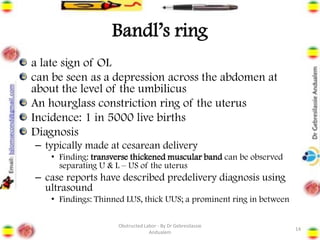
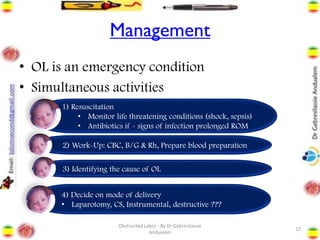
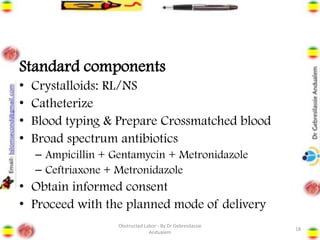
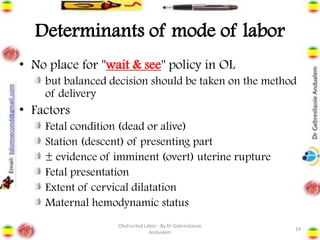
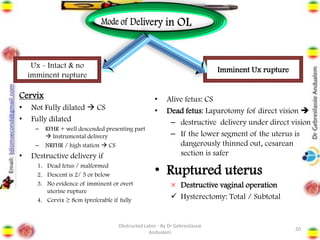
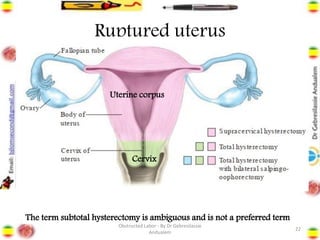
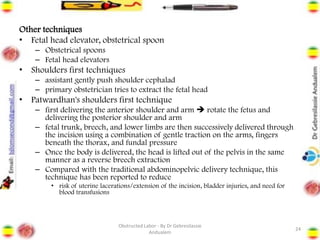
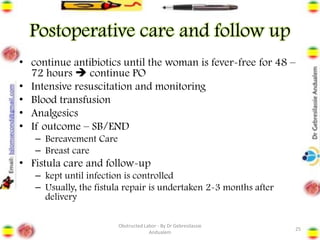
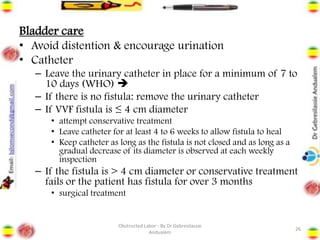
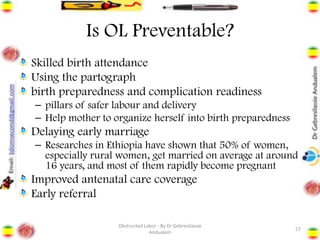
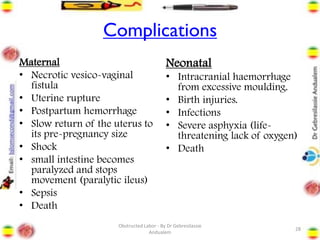
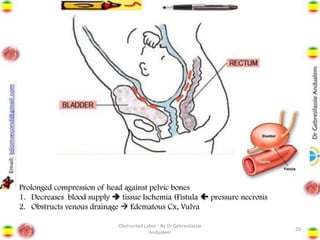
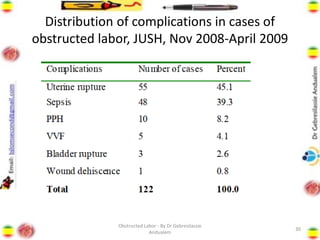
Obstructed labor is the failure of a fetus to progress down the birth canal due to mechanical reasons despite adequate contractions, making it a preventable complication. It represents a significant maternal and neonatal health risk, accounting for a notable percentage of maternal deaths, particularly in developing regions. Management requires prompt action, resuscitation, and a careful decision on the mode of delivery, with numerous associated complications if left unaddressed.