This document discusses various aspects of medication administration including:
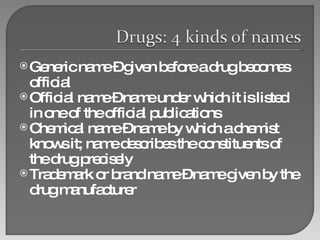
1. It defines key medication terminology such as generic names, official names, chemical names, and brand names.
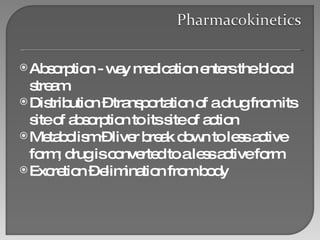
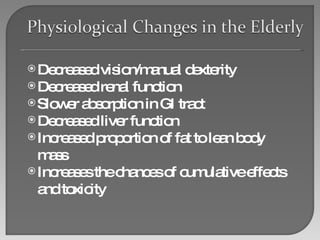
2. It describes the processes of absorption, distribution, metabolism, and excretion that medications undergo in the body.
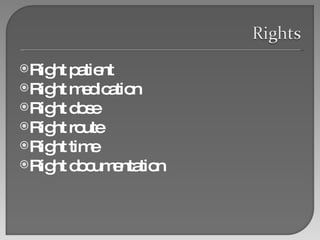
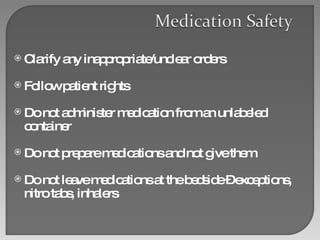
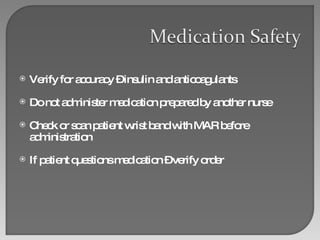
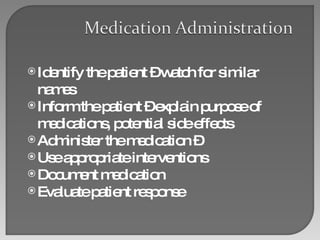
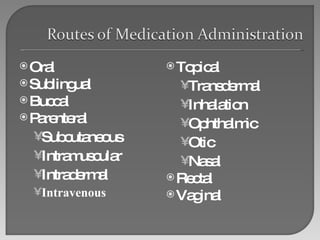
3. It lists important considerations for ensuring safe medication administration including the right patient, right medication, right dose, right route, and right documentation.