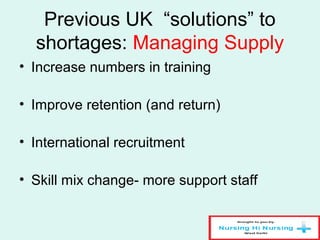
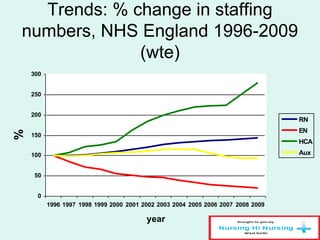
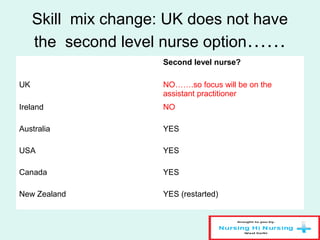
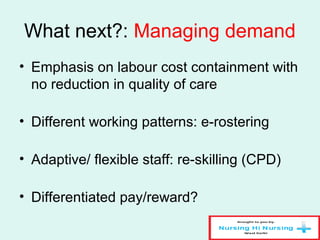
Nursing shortages are a complex issue influenced by factors like nurse supply and demand imbalances, gender discrimination, and links between nurse staffing levels and patient outcomes. While the UK has historically responded to shortages by increasing nurse training numbers and international recruitment, the future focus will likely shift to managing healthcare demand and changing nurse skill mix through roles like assistant practitioners to better utilize the nursing workforce. International comparisons show variation in nurse levels and wages across countries.
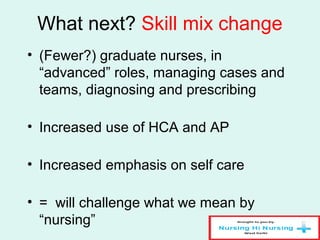
![Shortages: what we know
• There is no universal definition of a nursing shortage;
increasing evidence of nurse supply/ demand imbalances in
many countries. Imbalances can be organisational, specialty
based, regional, national ……(cyclical-”boom and bust”)
• Supply of nurses in many countries, low income and high
income, is failing to keep pace with increasing demand [e.g.
Sub-Saharan African countries = shortfall of + 600,000 nurses
in relation to Millennium Development Goals targets]
• Gender-based discrimination continues in many countries =
nursing undervalued as “women’s work”.
• There is a link between adequate nurse staffing levels and
positive care outcomes.](https://image.slidesharecdn.com/nursingshortages-140609032655-phpapp02/85/Nursing-shortages-4-320.jpg)
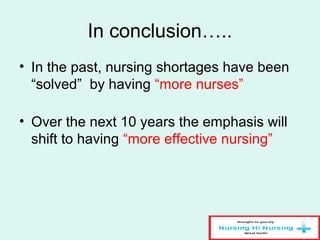
![UK and nursing shortages
• National policy control [£] of “supply”=
• =How many “new” nurses to train
• =What they are trained in……
• =How many nurses to employ in NHS/ how
much to pay them
• =How much £ to invest in their re-skilling
• =How many non EU nurses to allow into UK
• =when NHS nurses can retire…….](https://image.slidesharecdn.com/nursingshortages-140609032655-phpapp02/85/Nursing-shortages-5-320.jpg)