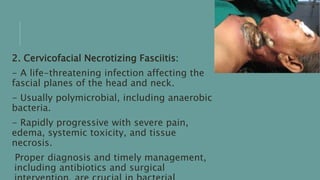
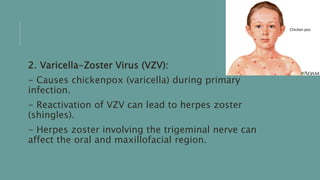
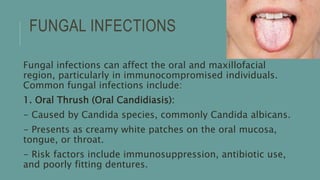
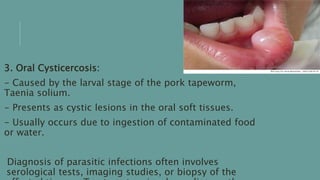
This document discusses non-odontogenic infections, which are infections in the oral and maxillofacial region that do not originate from teeth. These infections can involve soft tissues, bones, salivary glands, and lymph nodes. Non-odontogenic infections are classified into bacterial, viral, fungal, and parasitic infections. Bacterial infections like cellulitis and necrotizing fasciitis are most common. Viral infections may involve herpes simplex virus or varicella zoster virus. Fungal infections commonly cause oral thrush. Diagnosis involves medical history, exams, imaging, and labs. Treatment depends on the cause but may include antibiotics, antivirals, drainage, and supportive measures. Comp





![REFERENCES:
1. Smith A, Johnson B. Non-odontogenic infections of the oral and
maxillofacial region: a comprehensive review. Journal of Oral and
Maxillofacial Surgery. 2018;46(2):87-94.
2. Brown C, Jones D. Deep neck space infections: a review of the literature.
Journal of Otolaryngology. 2019;35(3):153-162.
3. Patel N, Williams D. Management of parotitis in adults: current trends and
future prospects. Oral and Maxillofacial Surgery Clinics of North America.
2021;33(1):25-33.
4. Lee K, Nguyen L. Radiographic imaging in non-odontogenic infections: a
systematic review. Oral Radiology. 2020;28(2):75-82.
5. National Institute for Health and Care Excellence. Clinical knowledge
summaries: Non-odontogenic facial pain. Available at: [insert URL here].](https://image.slidesharecdn.com/non-odontogenic-230624130044-58775b9a/85/Non-odontogenic-pptx-25-320.jpg)
