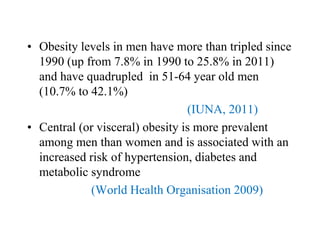
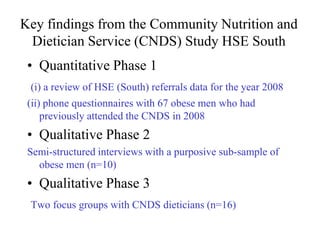
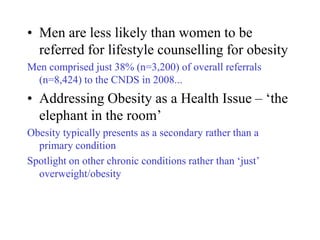
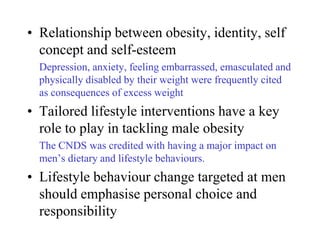
This document discusses perspectives on research and policy regarding weight loss and obesity in men's health. It provides an overview of why focusing on men is important, applying a gendered lens to male obesity, findings from a study on men referred to community nutrition and dietetic services, and best practice guidelines for tackling male obesity in primary care settings. Key points include that obesity levels in Irish men have sharply increased, men are less likely to see their weight as a concern and seek help, and primary care approaches should emphasize physical activity, practical strategies, and long-term follow up for men.

![1. Men’s diets are less healthy than women’s
diets
2. Men who are overweight/obese tend not to
see their [excess] weight as a cause of
concern
3. Men tend to lack control over their diets
and are less knowledgeable about healthy
eating
4. Men’s dietary habits tend to be adversely
influenced by working unsociable hours
5. Men’s approach to food tends to be
pleasure-oriented](https://image.slidesharecdn.com/noelrichardson-110614070824-phpapp01/85/Noel-richardson-7-320.jpg)
![1. Don’t ignore the problem [of male obesity]
GPs have a crucial role to play
2. Adopt a ‘shared investment’ approach to
lifestyle change
3. Increase the breadth and capacity of
primary care teams to deal with obesity
Exercise referral, mental health & addiction services
4. Consider the impact of key ‘transitional’
periods in men’s lives
5. Account for and anticipate likely problems
or barriers to weight-loss](https://image.slidesharecdn.com/noelrichardson-110614070824-phpapp01/85/Noel-richardson-13-320.jpg)