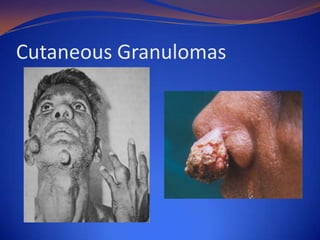
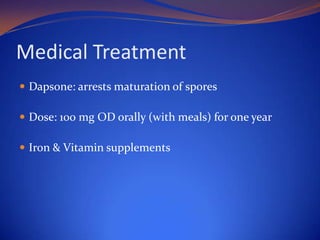
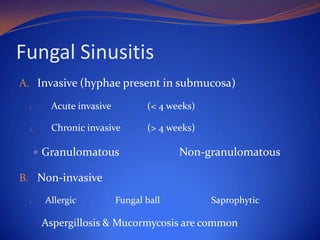
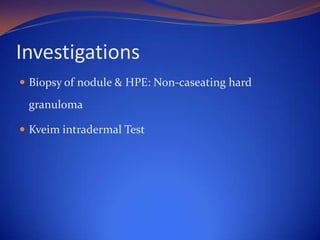
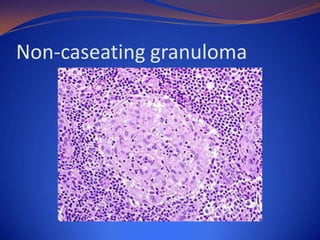
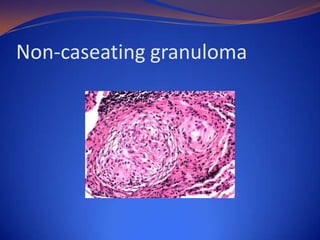
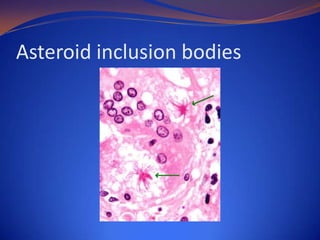
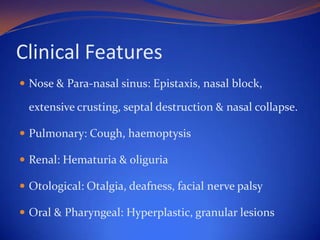
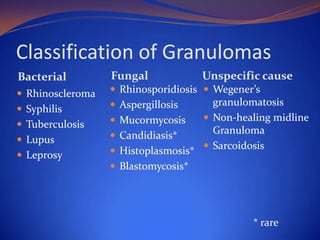
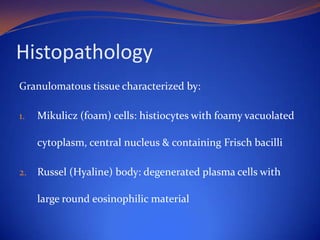
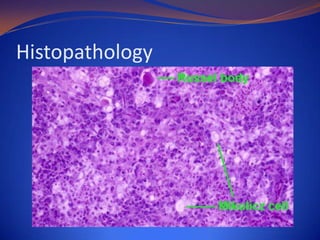
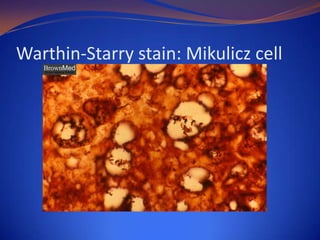
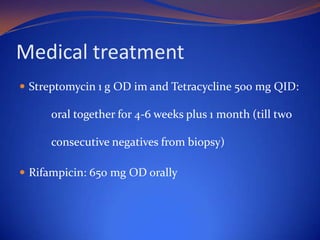
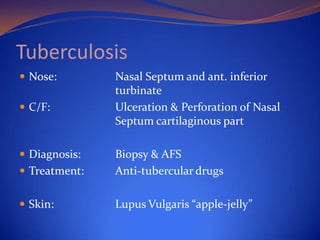
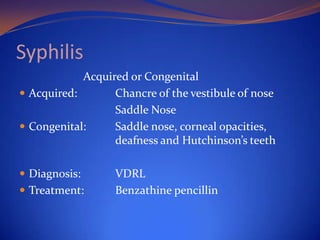
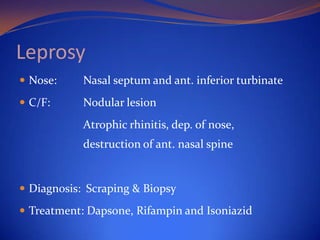
This document discusses granulomas and provides classifications and definitions. It defines a granuloma as a tumor-like mass of nodular granulation tissue due to chronic inflammation. Granulomas are classified as bacterial, fungal, or of unspecified cause. Examples of bacterial granulomas include rhinoscleroma, syphilis, tuberculosis, and leprosy. Fungal granulomas include rhinosporidiosis, aspergillosis, mucormycosis, and candidiasis. Unspecific granulomas include Wegener's granulomatosis, non-healing midline granuloma, and sarcoidosis. The document then provides further details on specific granulomas such as

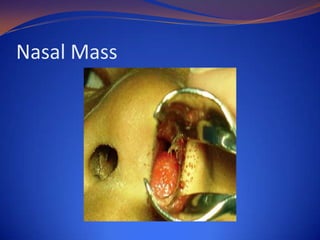
![Definition
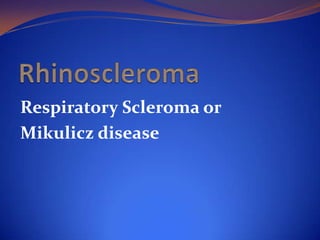
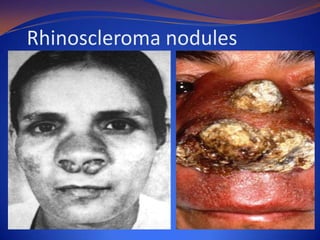
Rhinoscleroma or scleroma is a chronic granulomatous
disease caused by gram negative bacillus Klebsiella
rhinoscleromatis [von Frisch bacillus].](https://image.slidesharecdn.com/nasalgranulomas13-131204062118-phpapp02/85/Nasal-Granuloma-6-320.jpg)
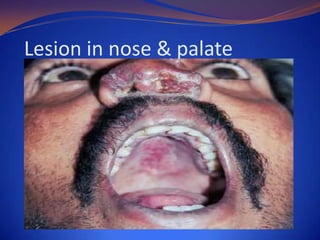


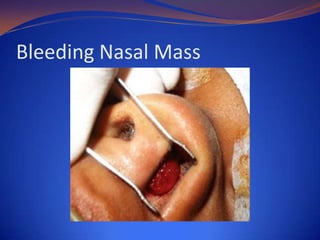
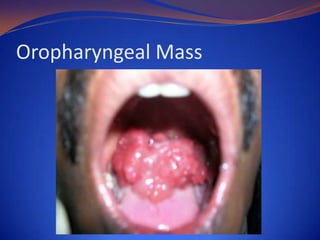
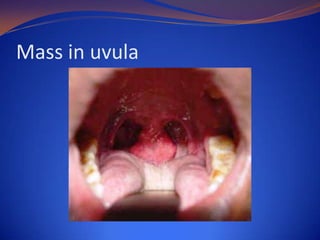
![Clinical Presentation
Epistaxis + nasal discharge + nose block
Nasal mass: papillomatous or polypoid, granular,
friable, bleeds on touch, pedunculated or sessile, pink
surface studded with white dots [Strawberry
appearance], involves septum & turbinates](https://image.slidesharecdn.com/nasalgranulomas13-131204062118-phpapp02/85/Nasal-Granuloma-26-320.jpg)