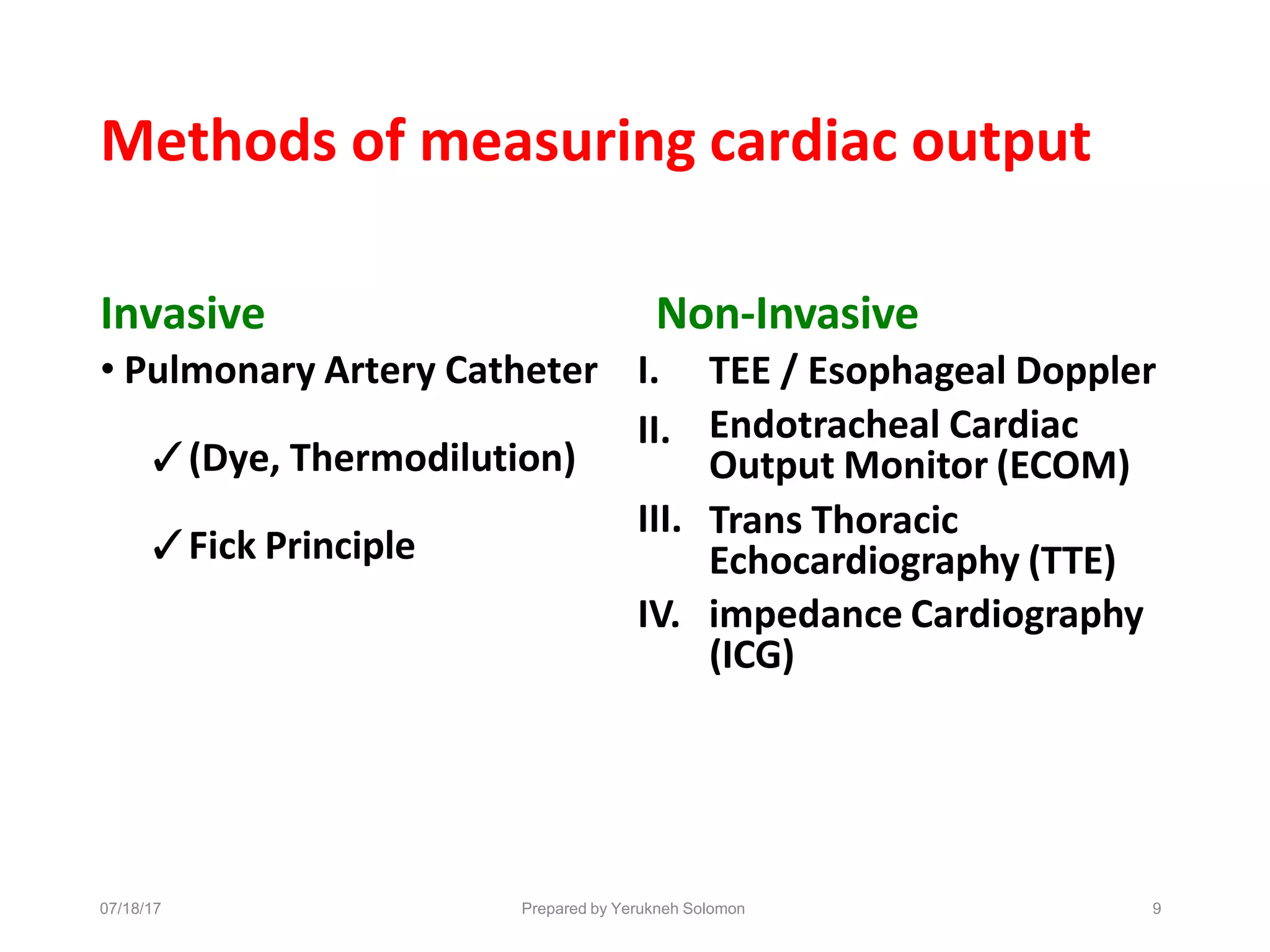
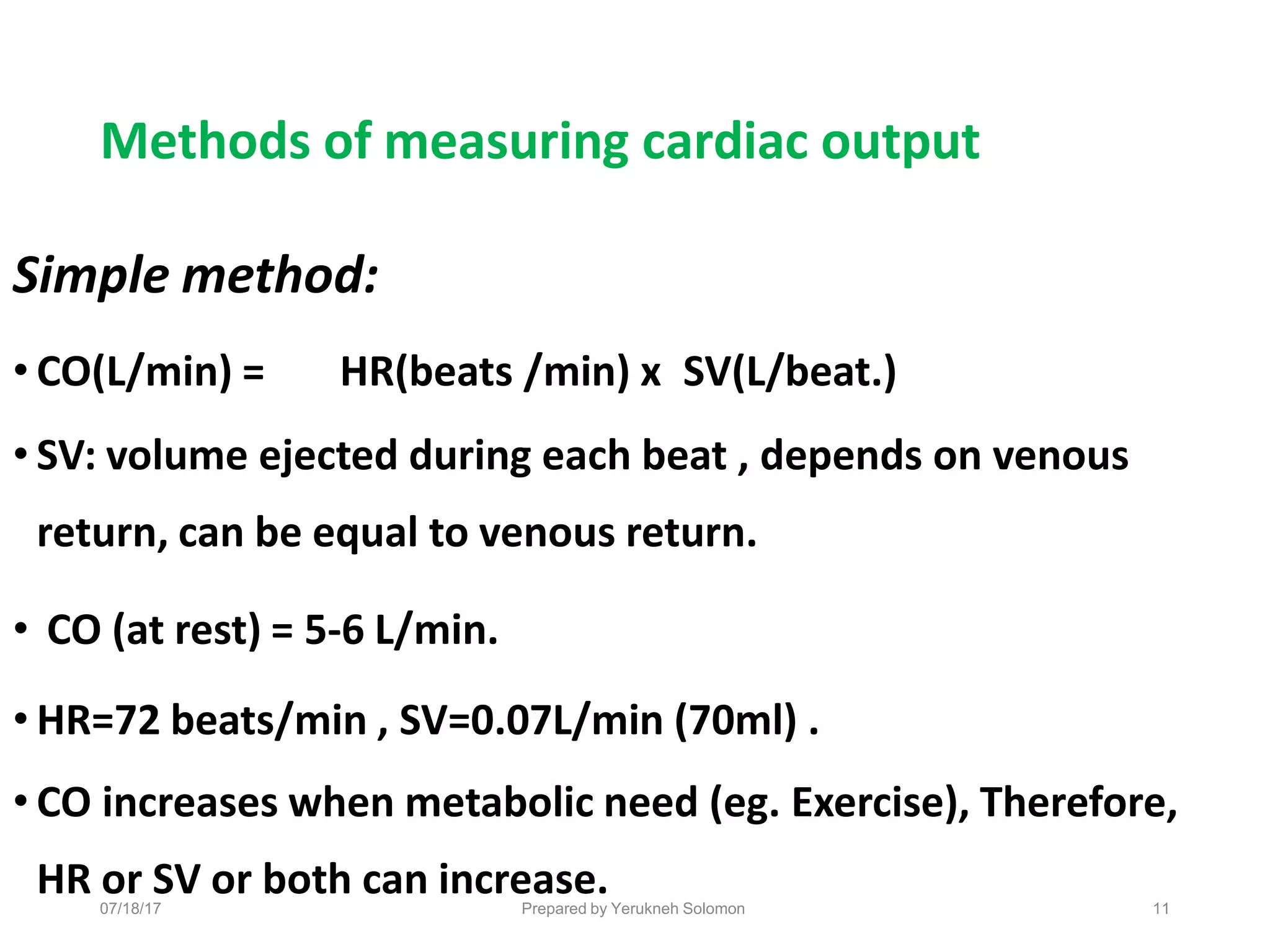
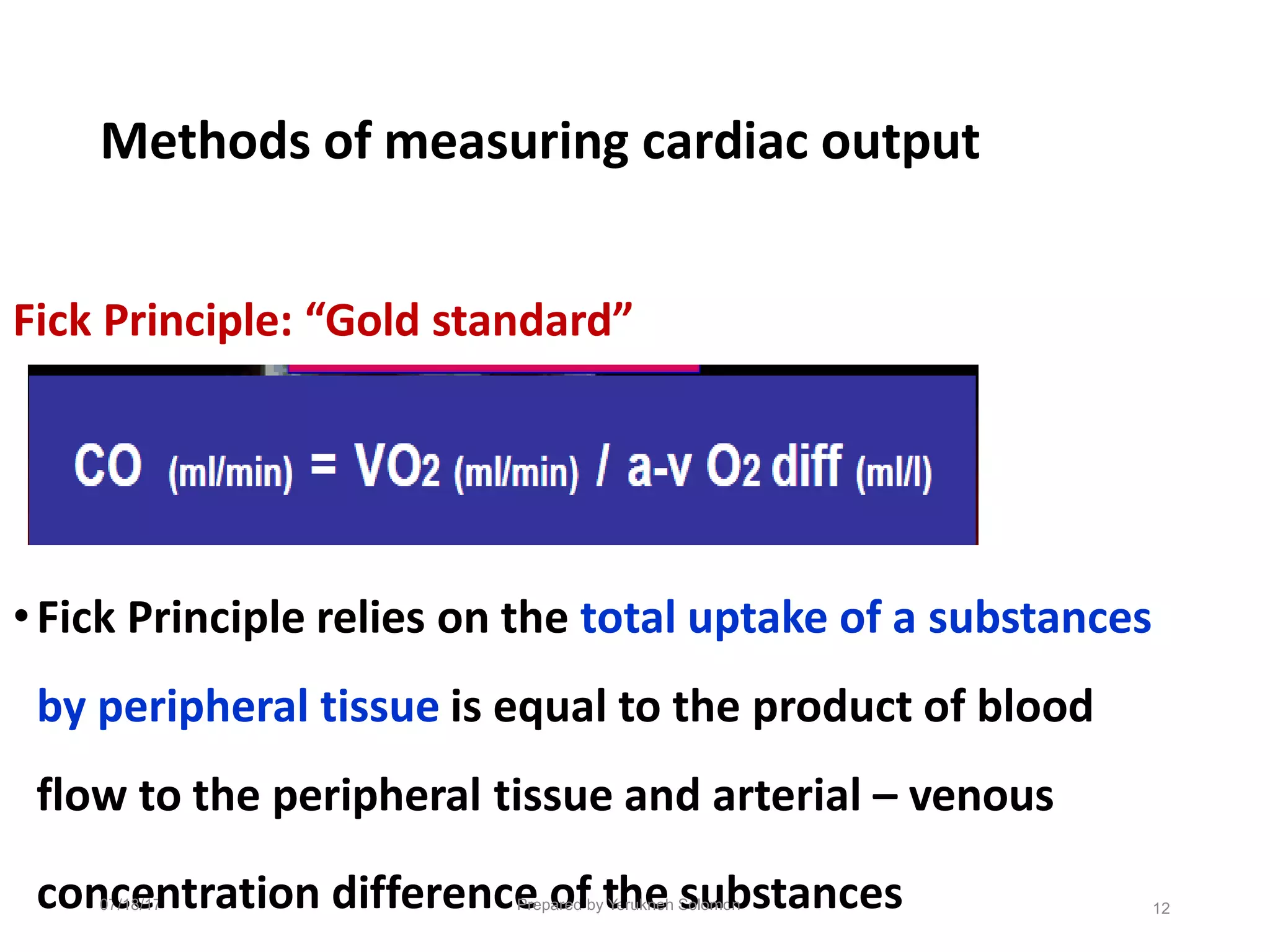
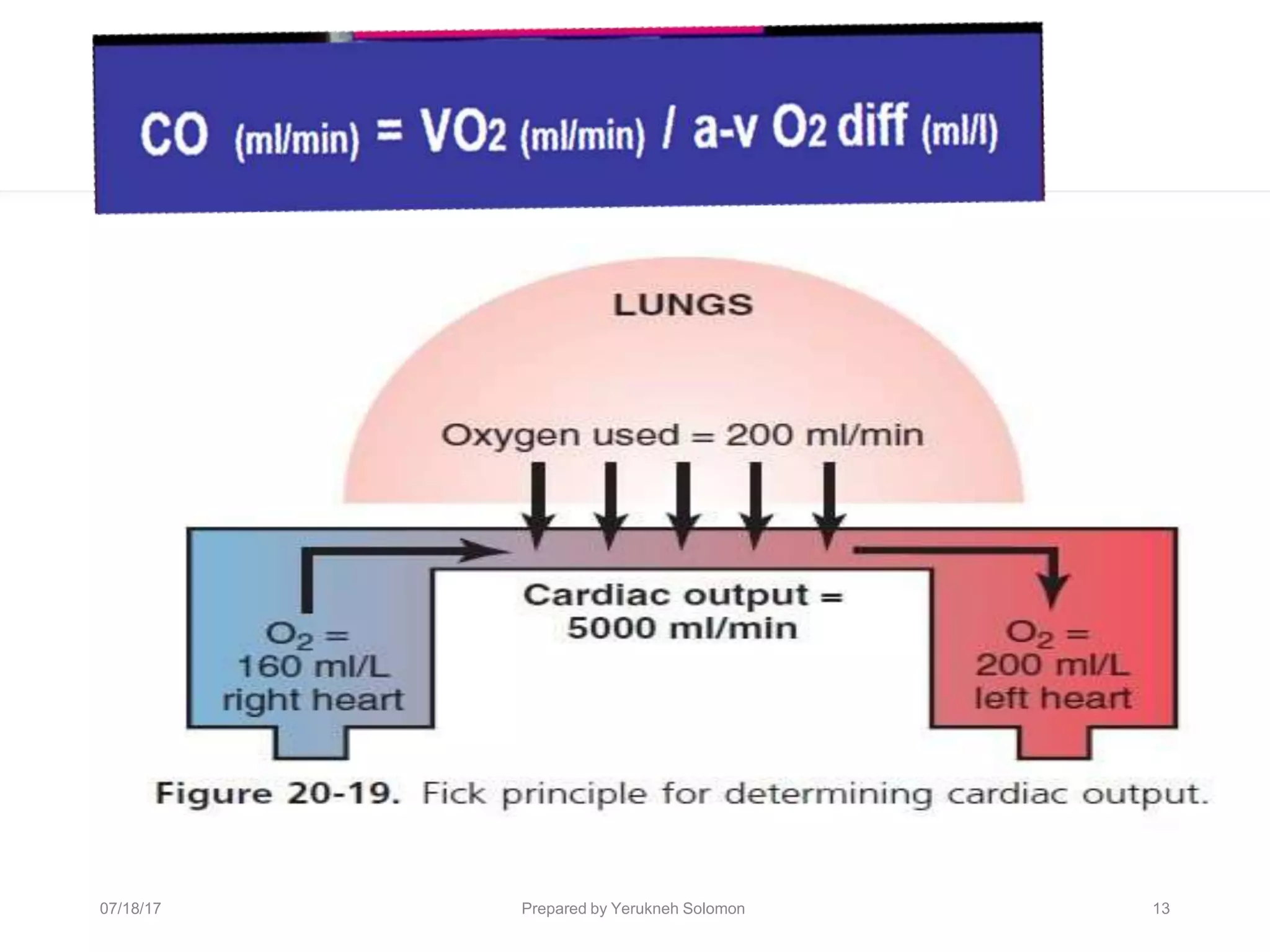
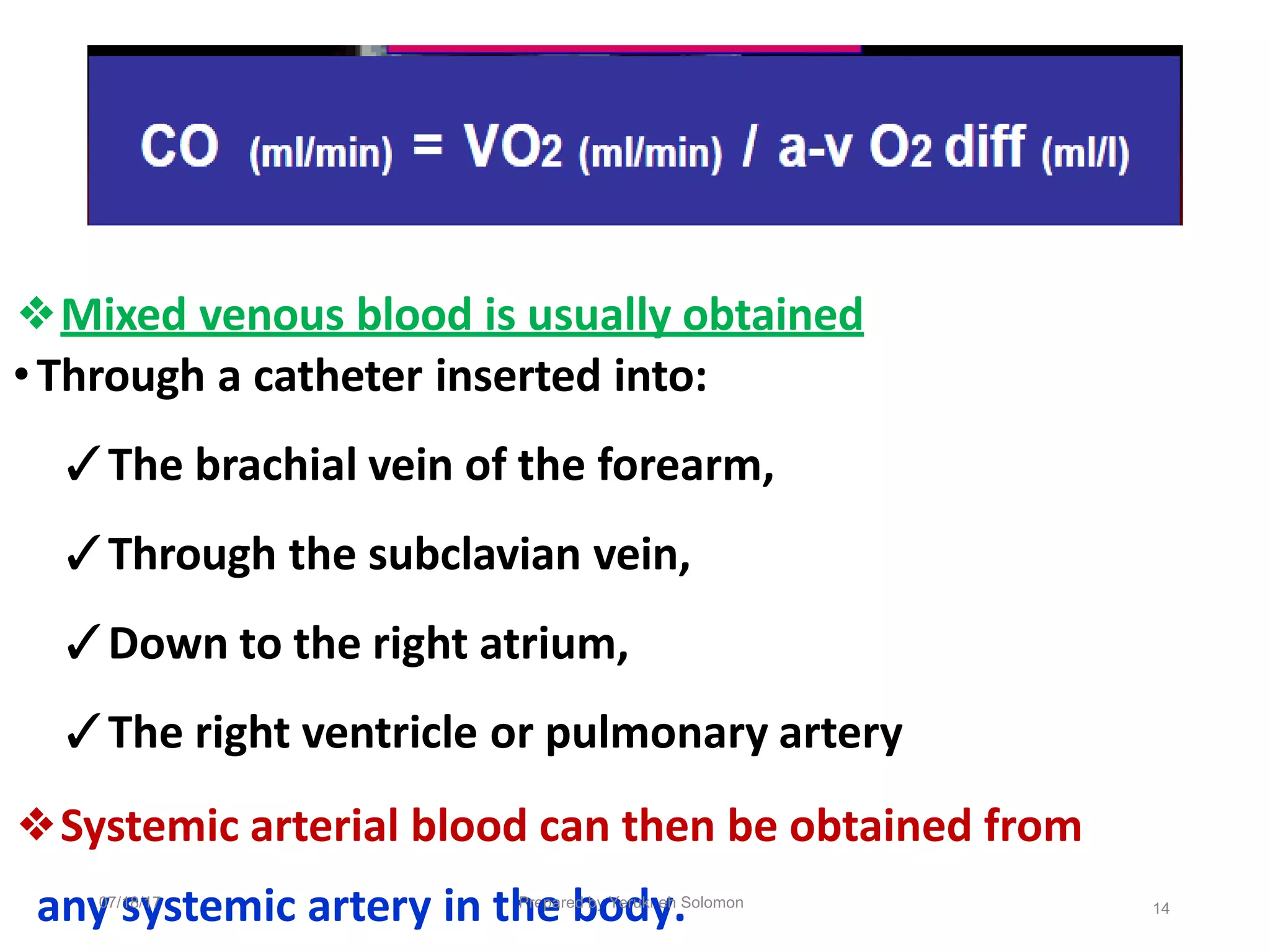
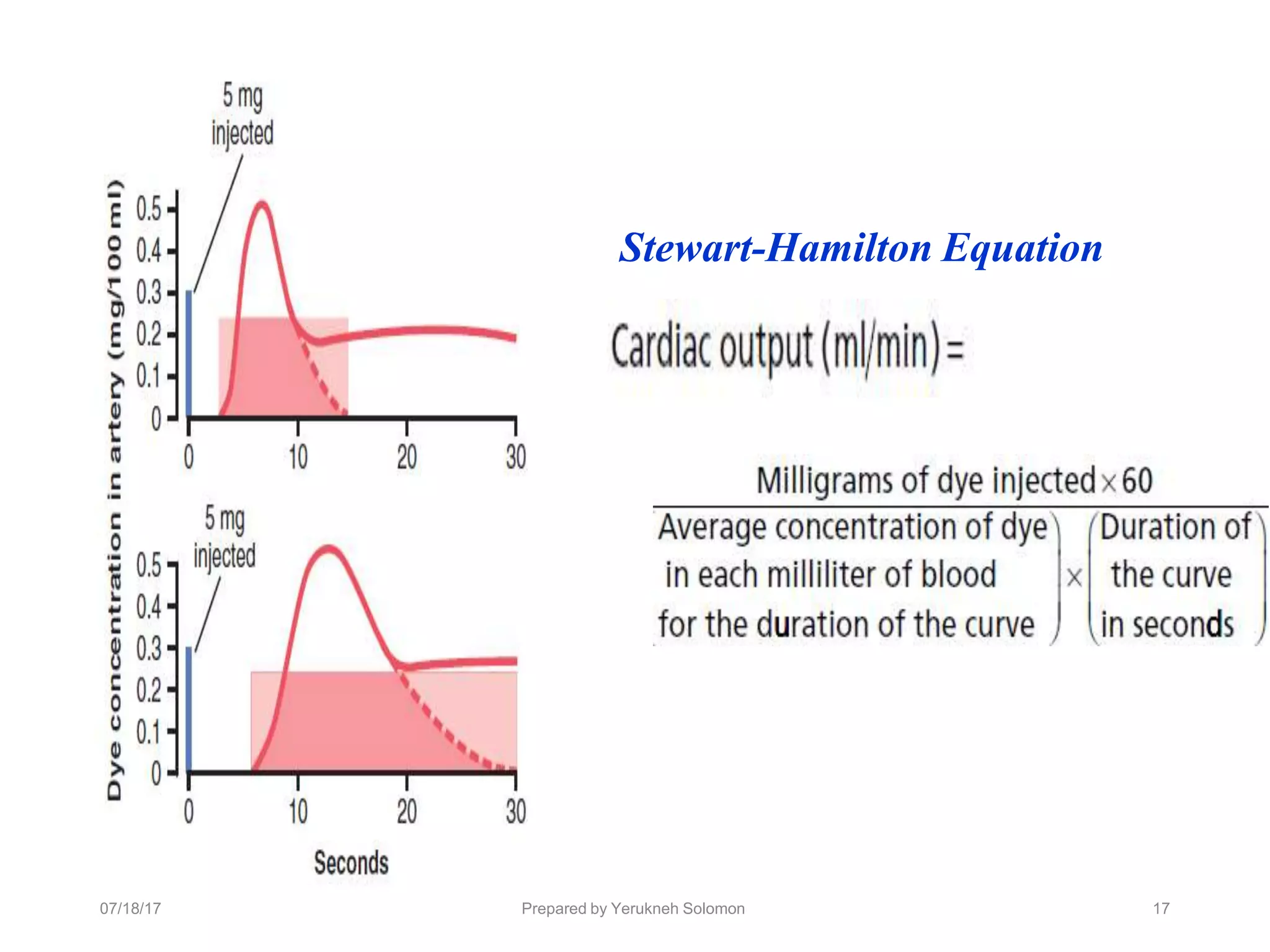
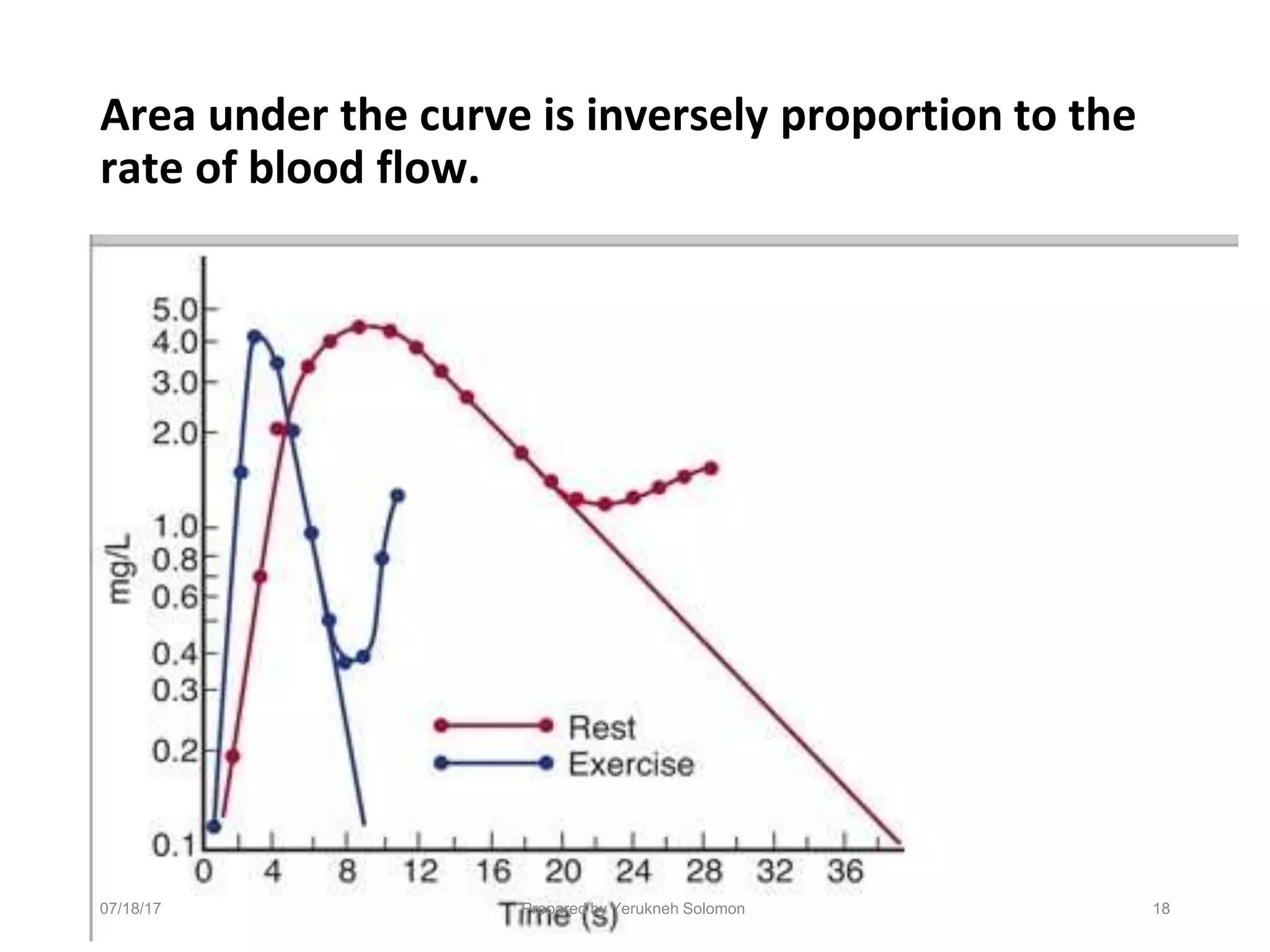
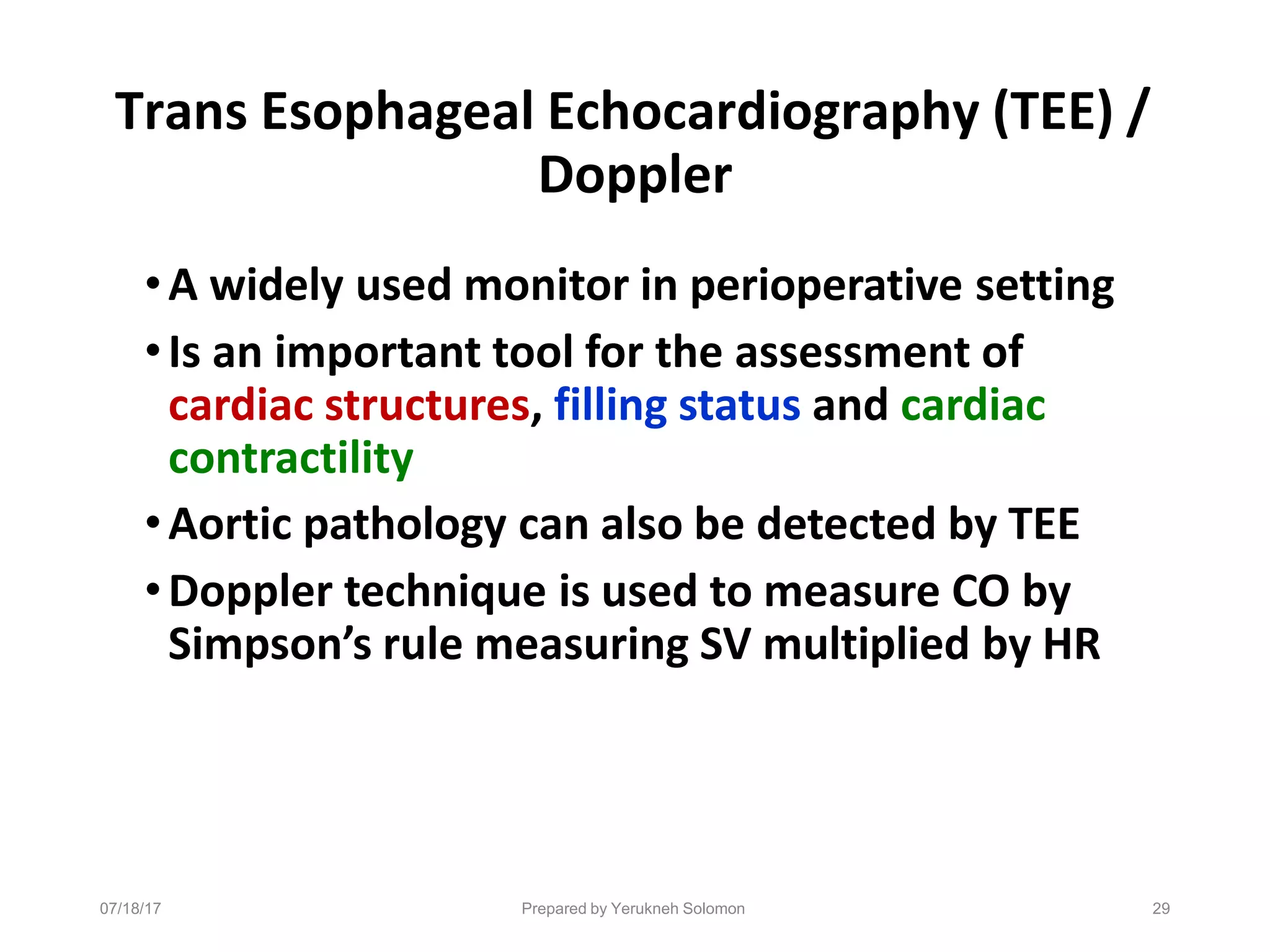
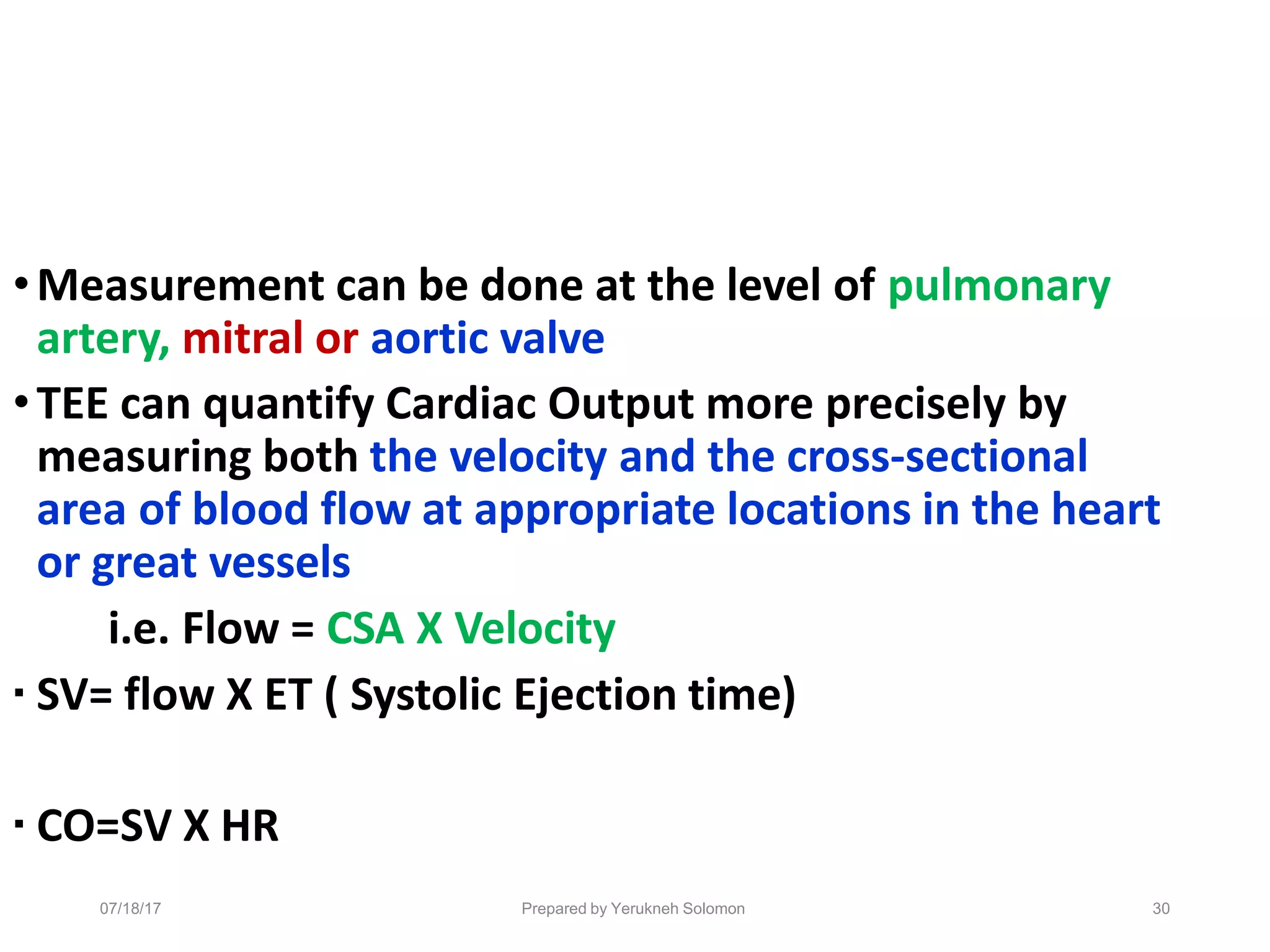
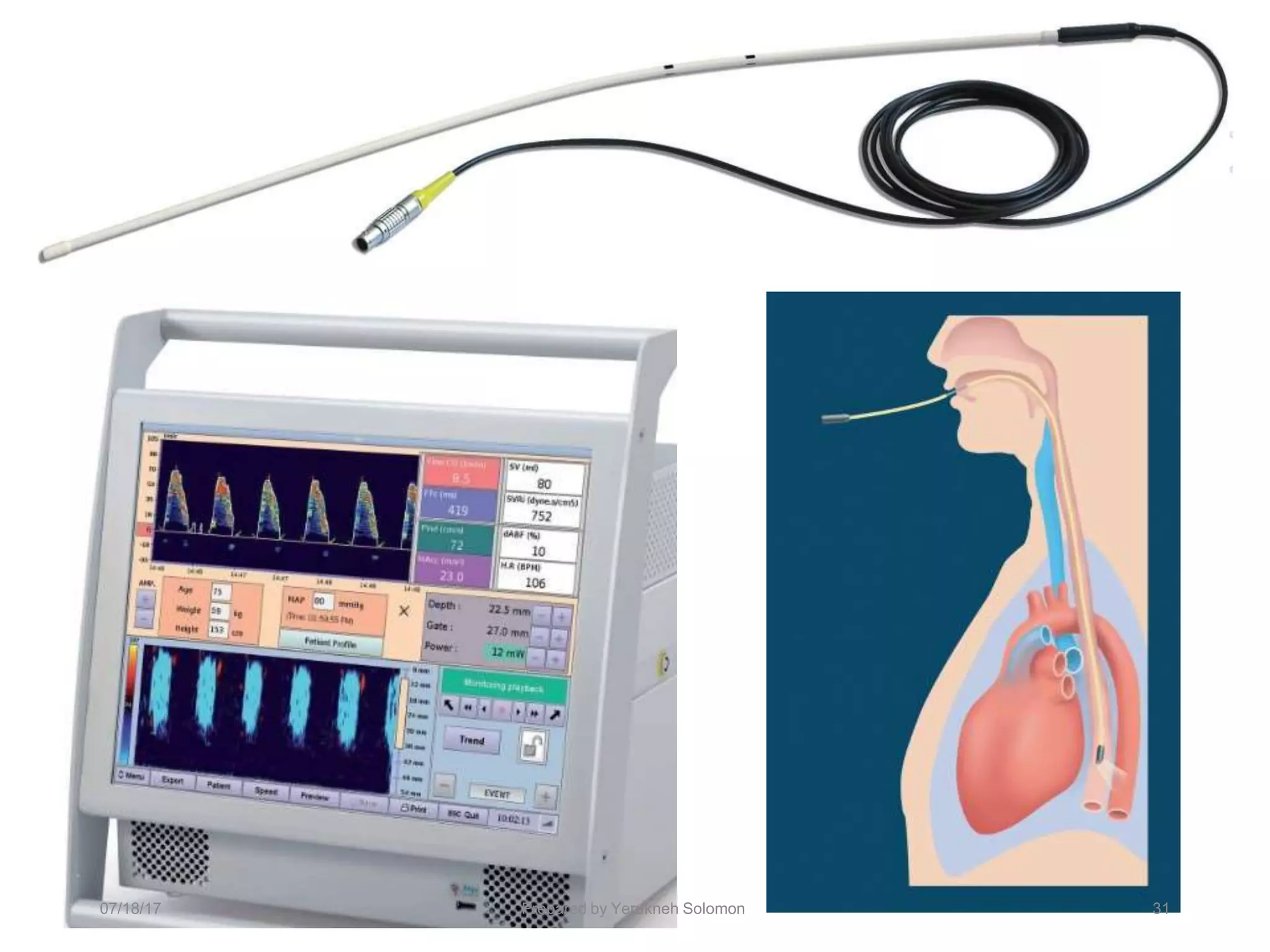
This document outlines various methods for measuring cardiac output. It begins with a historical perspective on cardiac output measurement, noting that Adolf Fick first developed a technique for measuring it in 1870 using what is now called the Fick principle. The document then discusses the importance of cardiac output and ideal features of measurement devices. It describes both non-invasive techniques like echocardiography and invasive methods like thermodilution that use indicator dilution. The relationship between cardiac output, stroke volume, heart rate and cardiac reserve is also explained.
![07/18/17 Prepared by Yerukneh Solomon 37
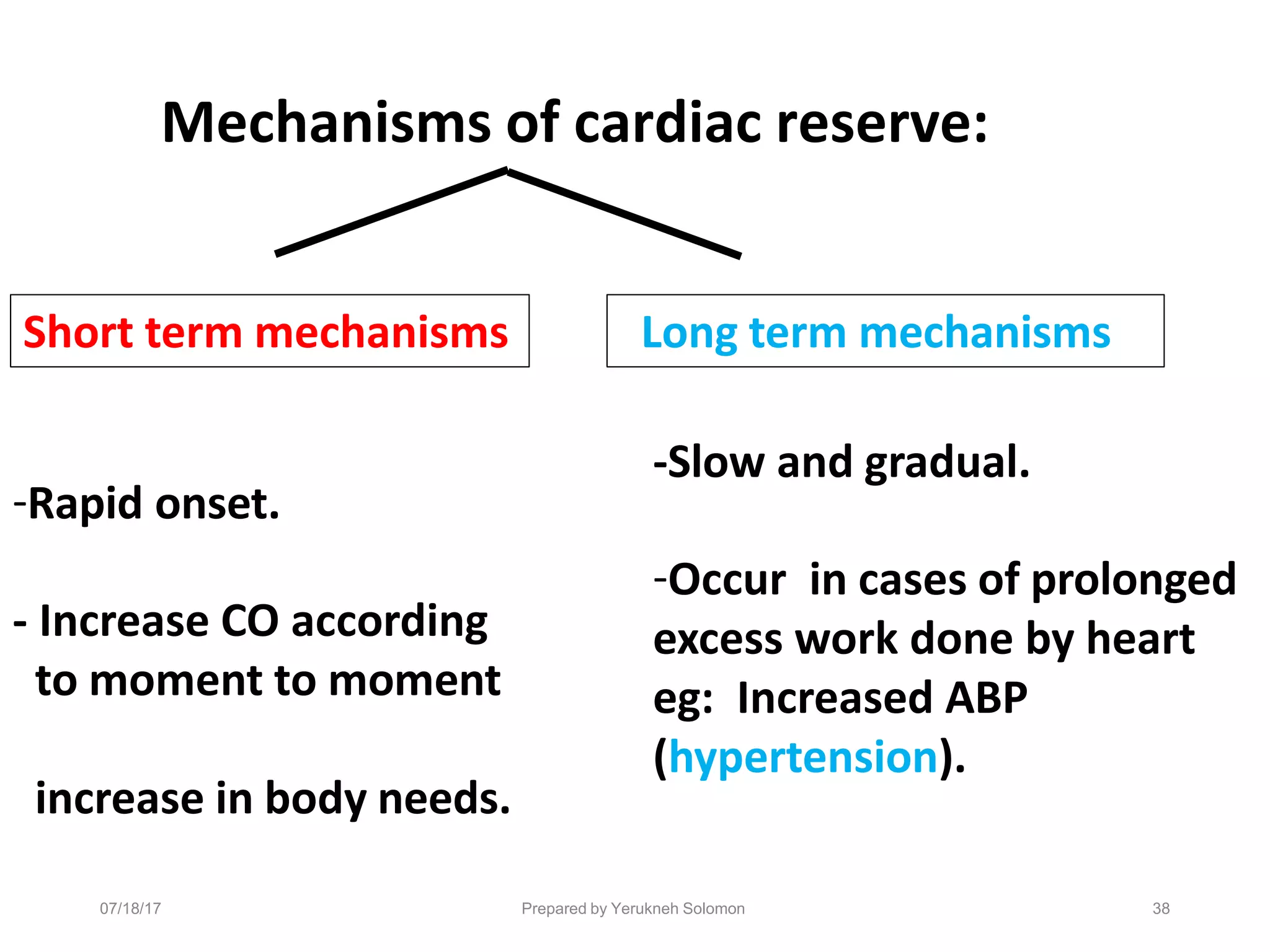
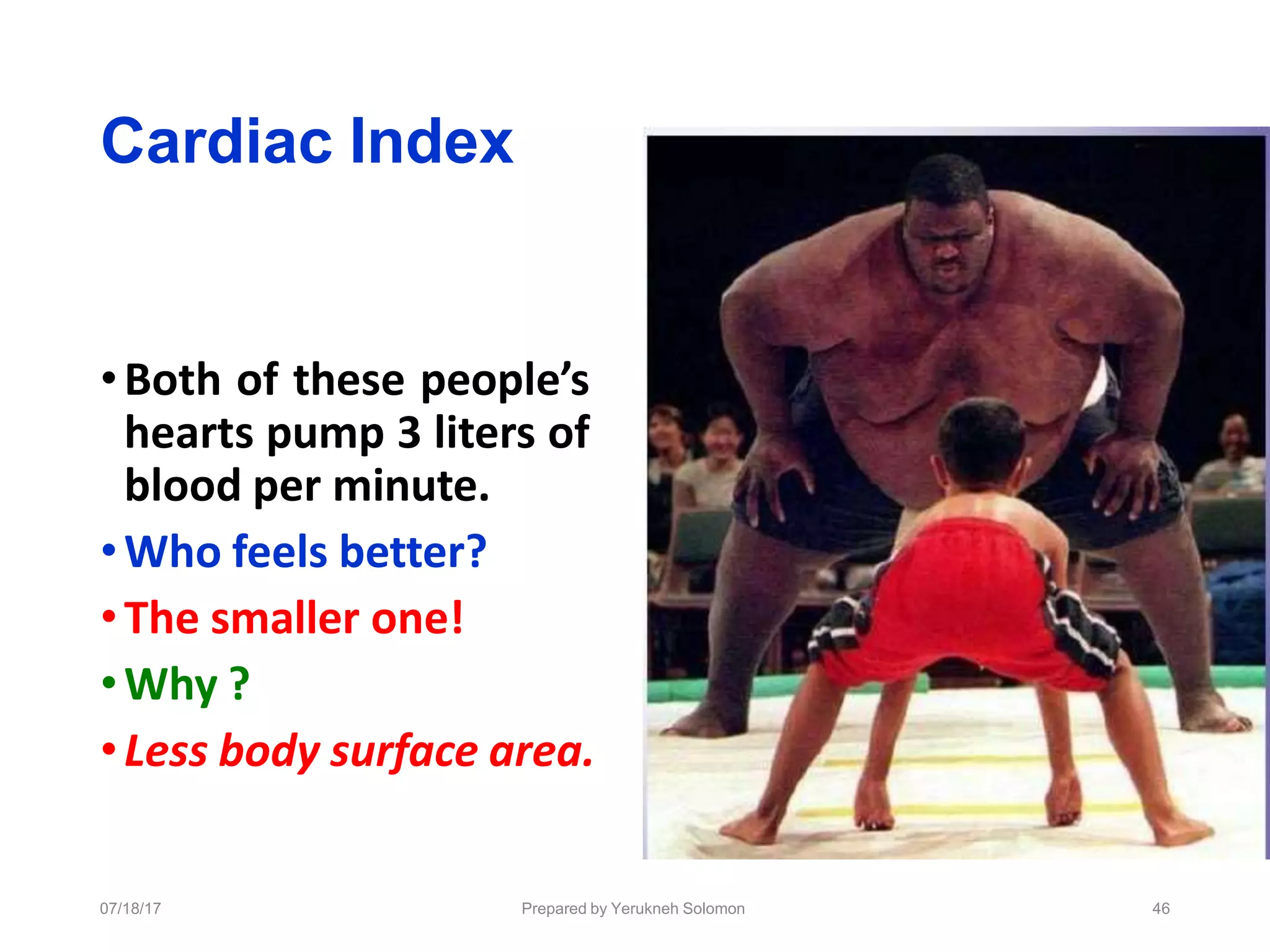
Cardiac reserve
•Cardiac reserve refers to the heart's ability to adjust to
the demands placed upon it.
❑Cardiac reserve =
[cardiac output during stress - cardiac output at rest.]
•In the normal young adult the resting cardiac output is
about 5-6 L/min and the cardiac reserve is nearly 30
L/min.](https://image.slidesharecdn.com/myassignment-1707180747521-230616182221-e16b34d6/75/myassignment-170718074752-1-pptx-37-2048.jpg)
![07/18/17 Prepared by Yerukneh Solomon 50
• Ganong’s Review of Medical Physiology - 23rdEd
• Medical physiology : a cellular and molecular approach /
[edited by] Walter F. Boron, Emile L. Boulpaep. 2nded.
• Guyton and hall textbook of medical physiology, 13th
edition
• http://heart.bmj.com/content/79/3/289#BIBL
• Chew MS, Aneman A. Haemodynamic monitoring using
arterial waveform analysis. Curr Opin Crit Care.
2013;19:234-41](https://image.slidesharecdn.com/myassignment-1707180747521-230616182221-e16b34d6/75/myassignment-170718074752-1-pptx-50-2048.jpg)