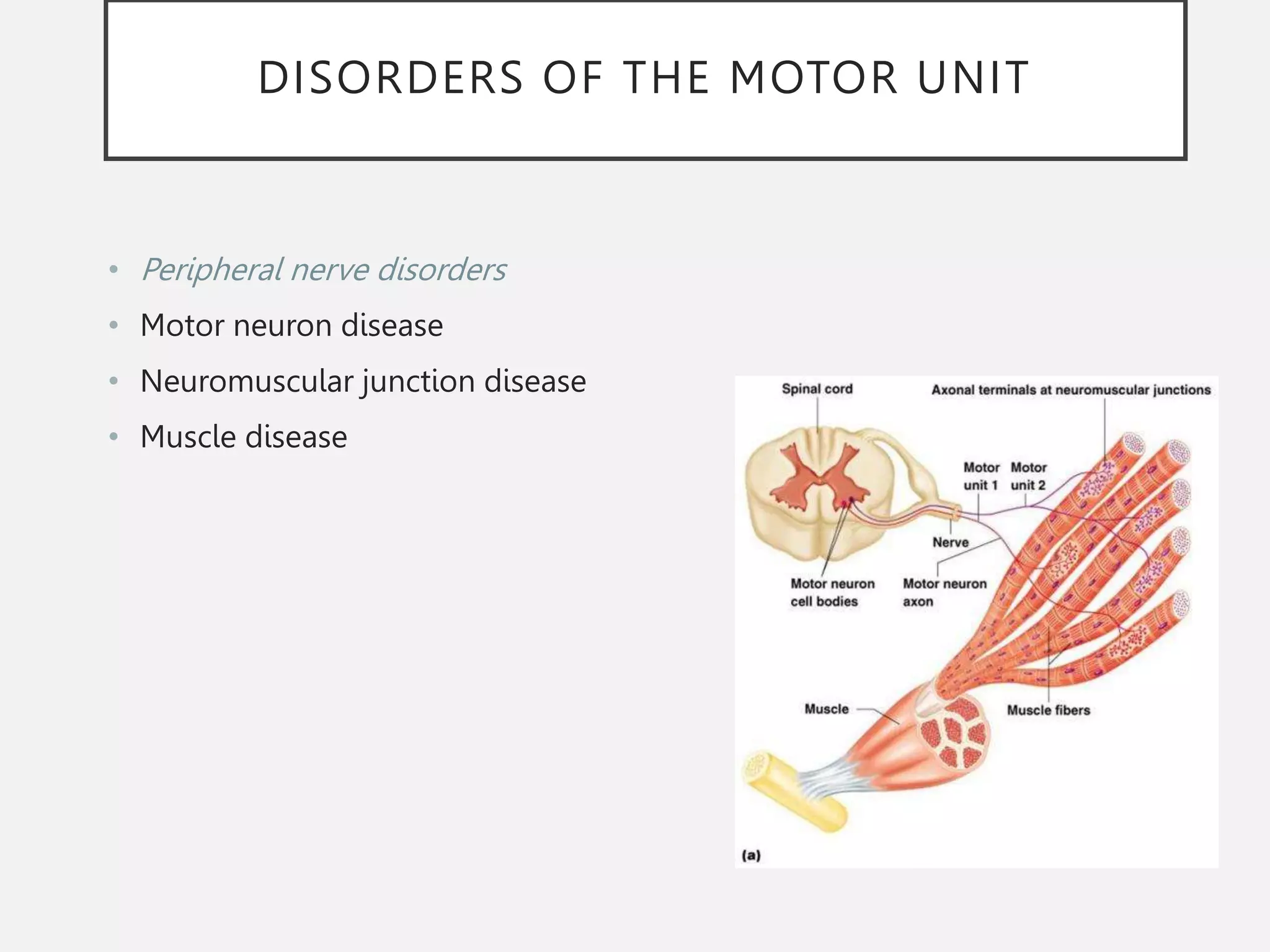
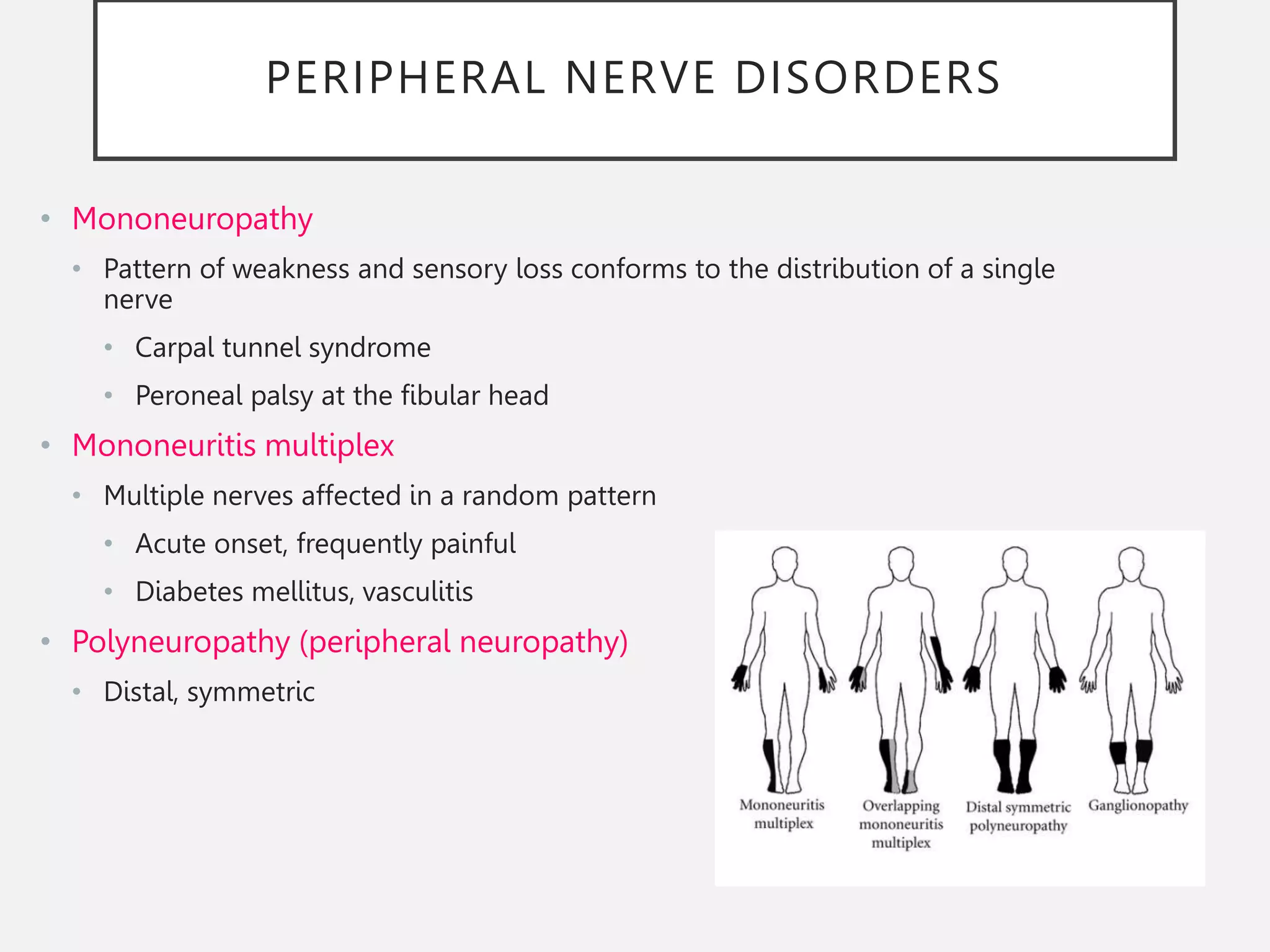
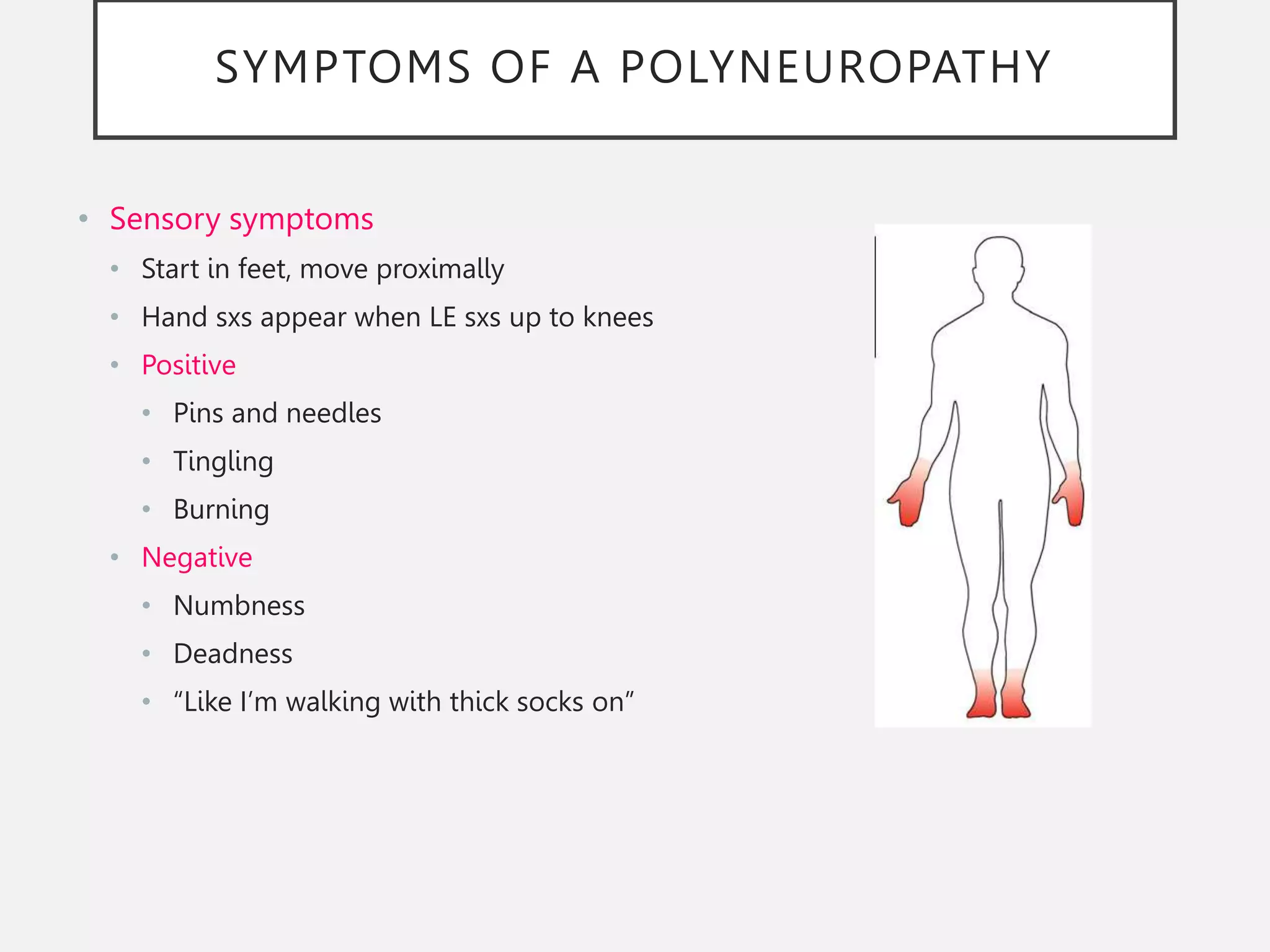
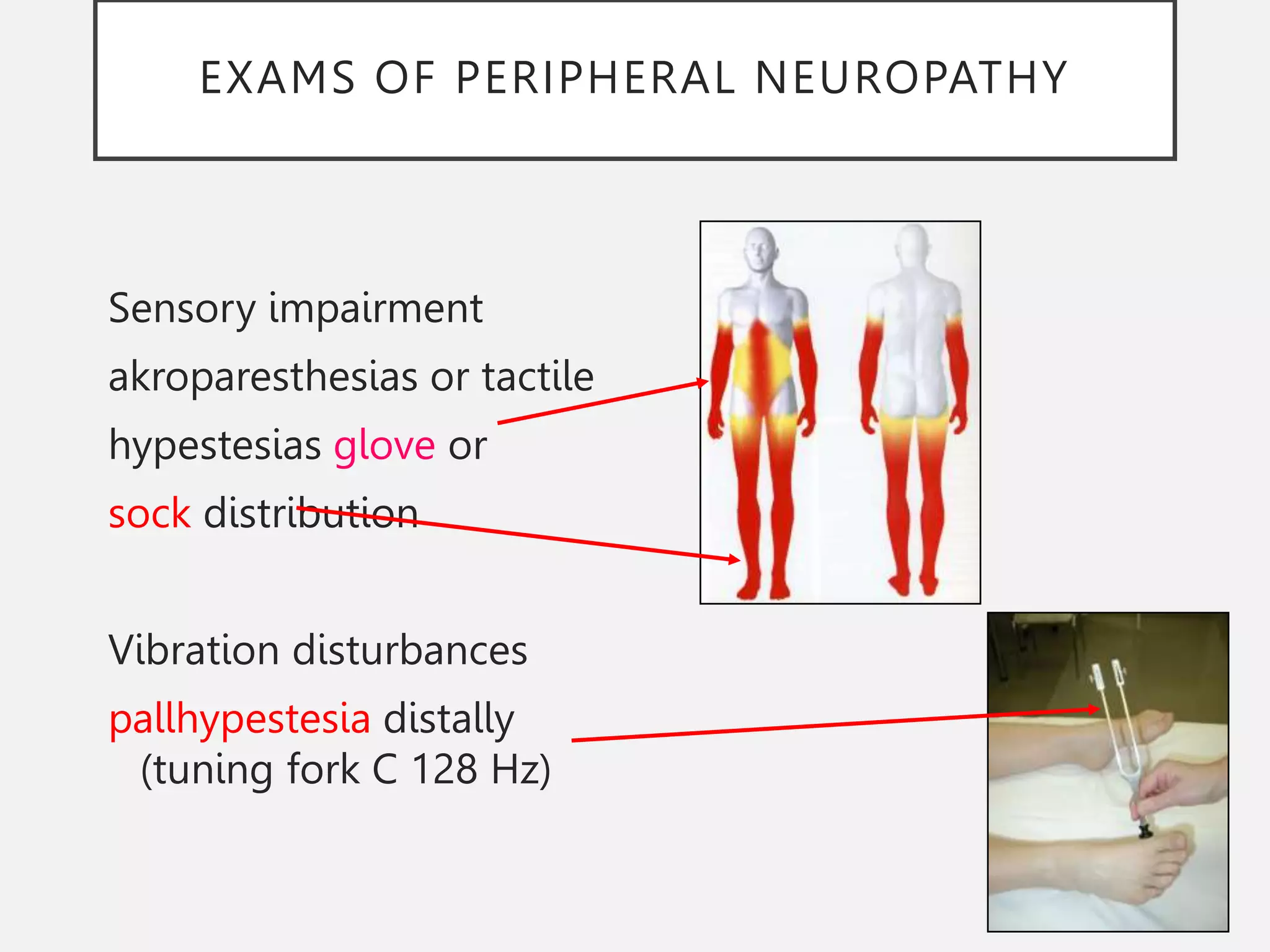
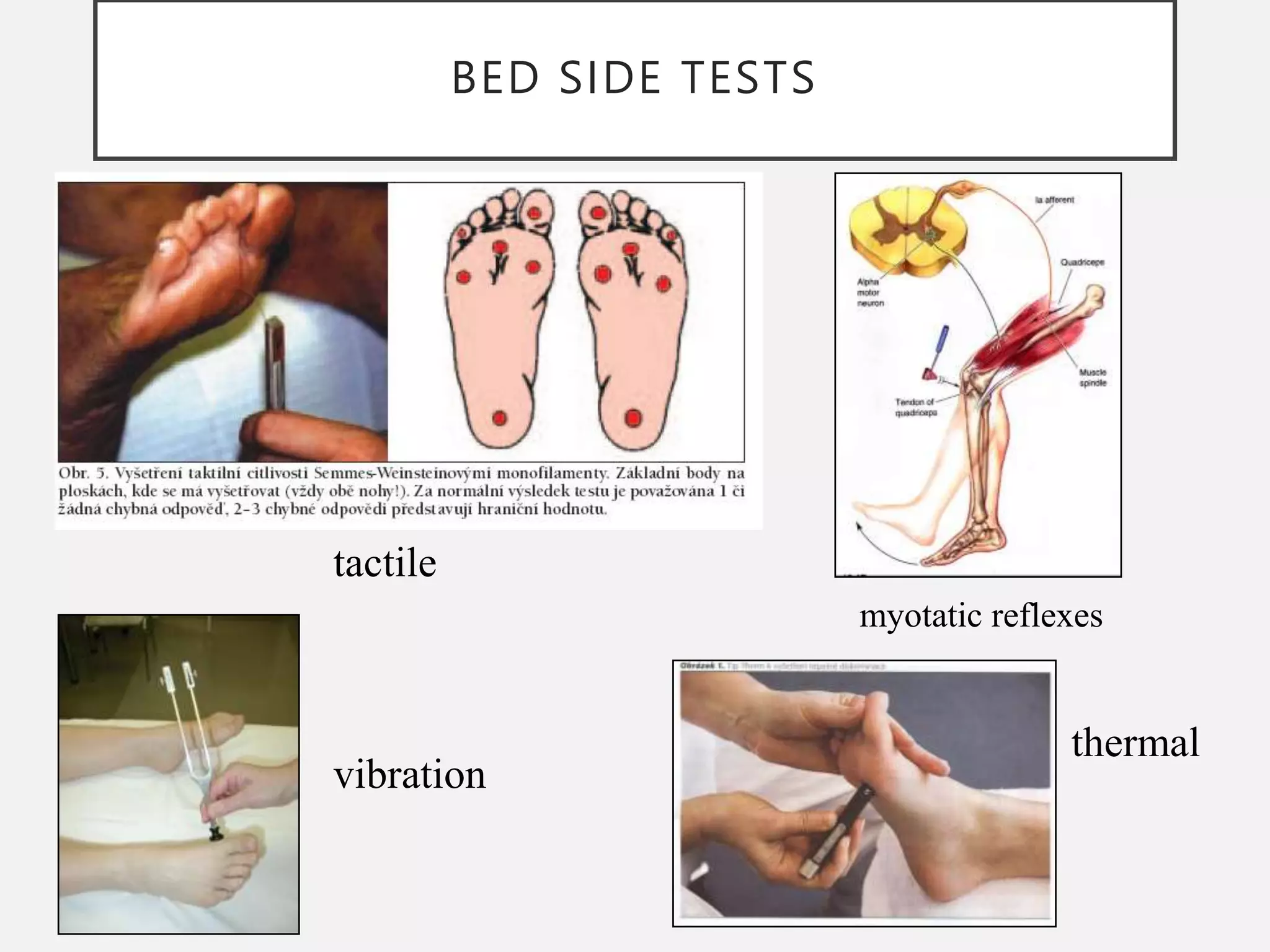
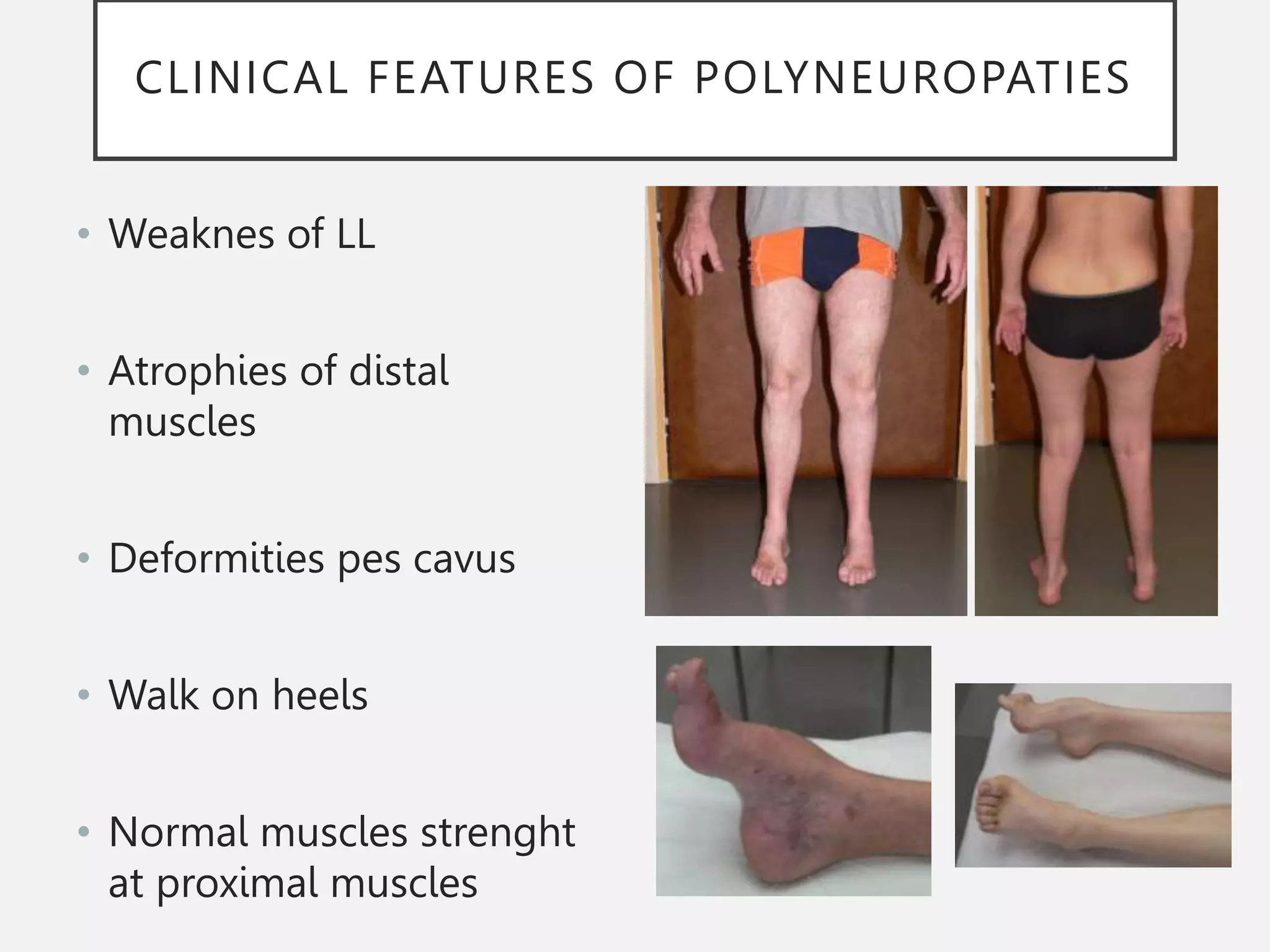
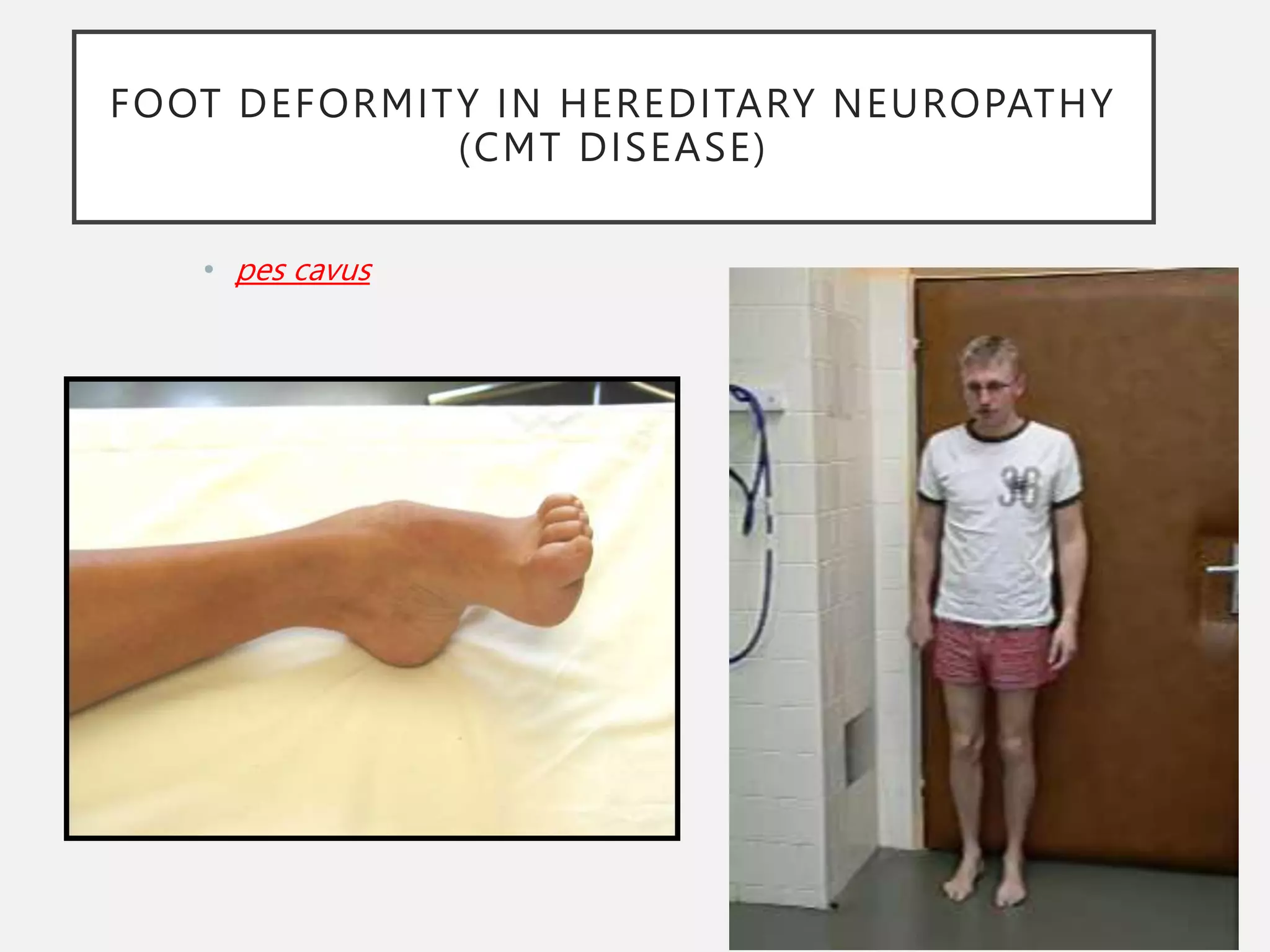
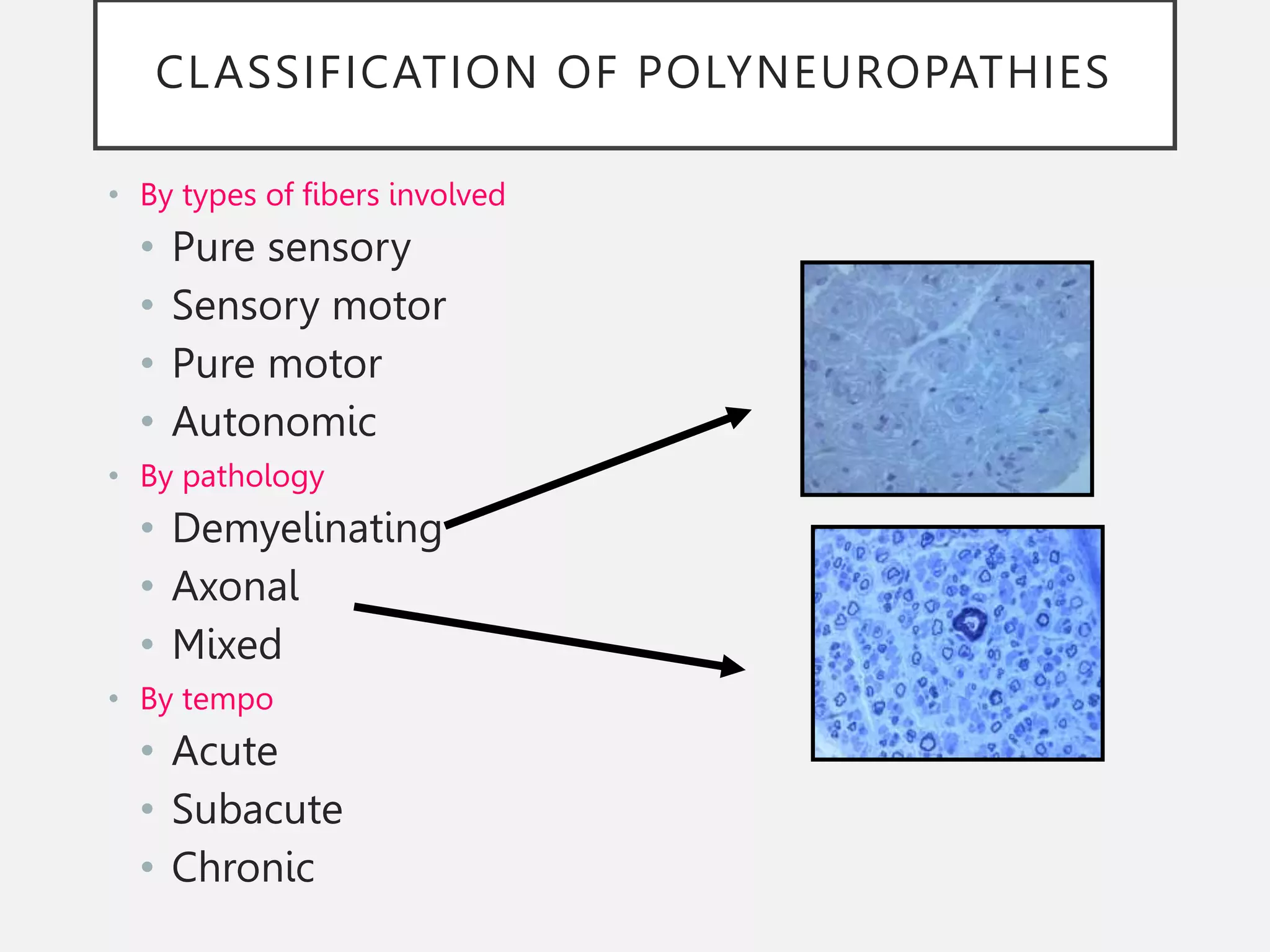
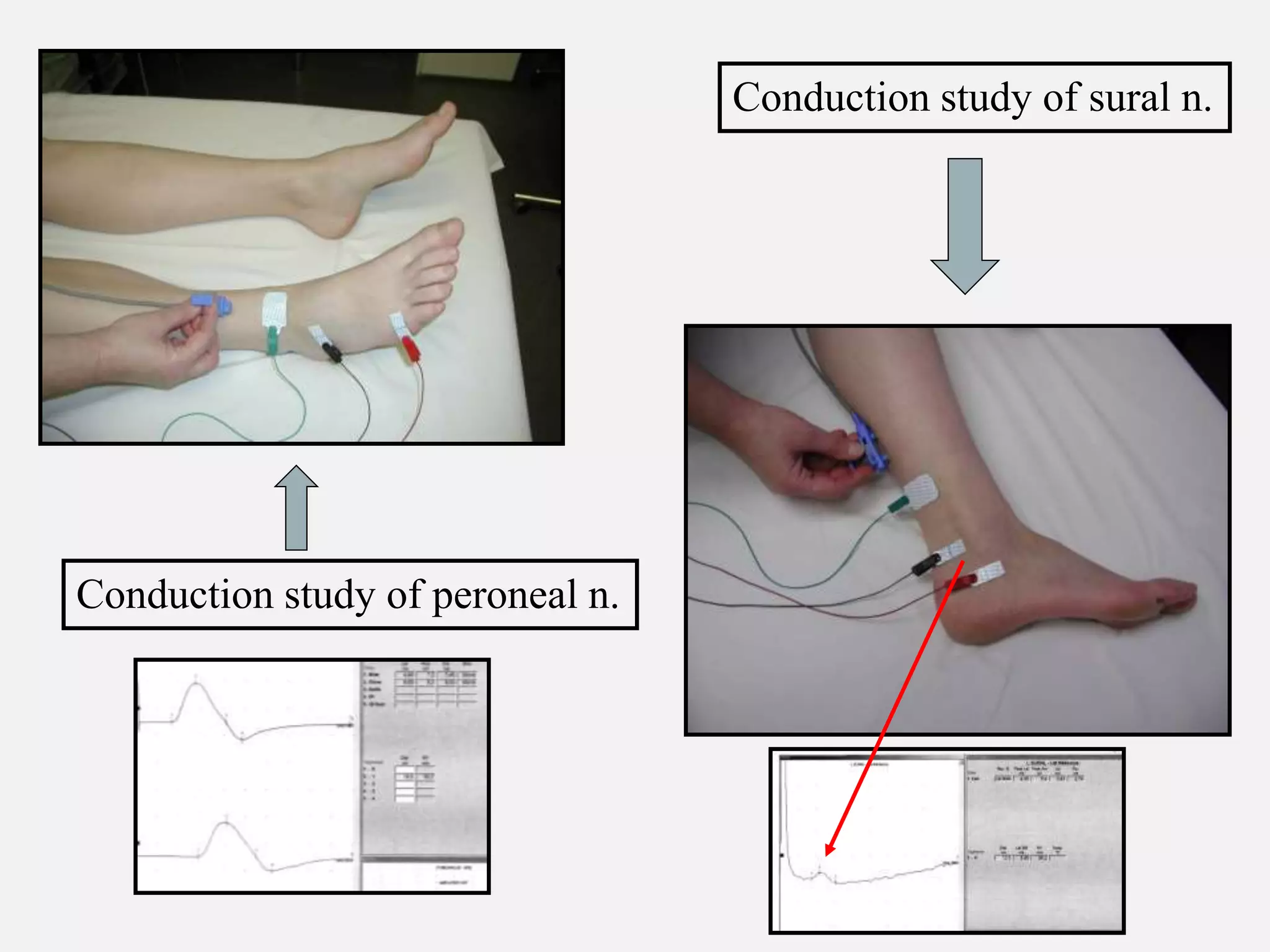
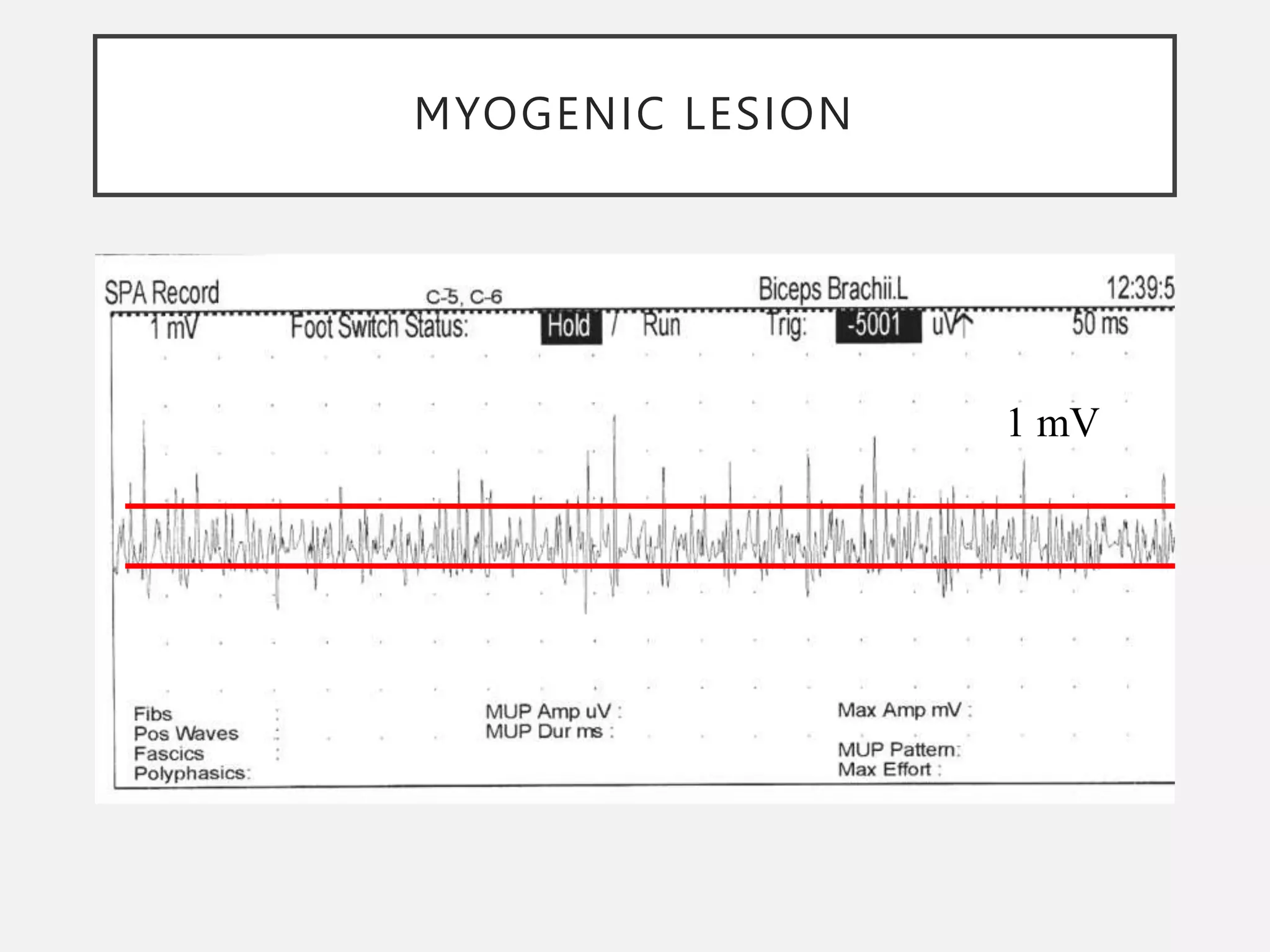
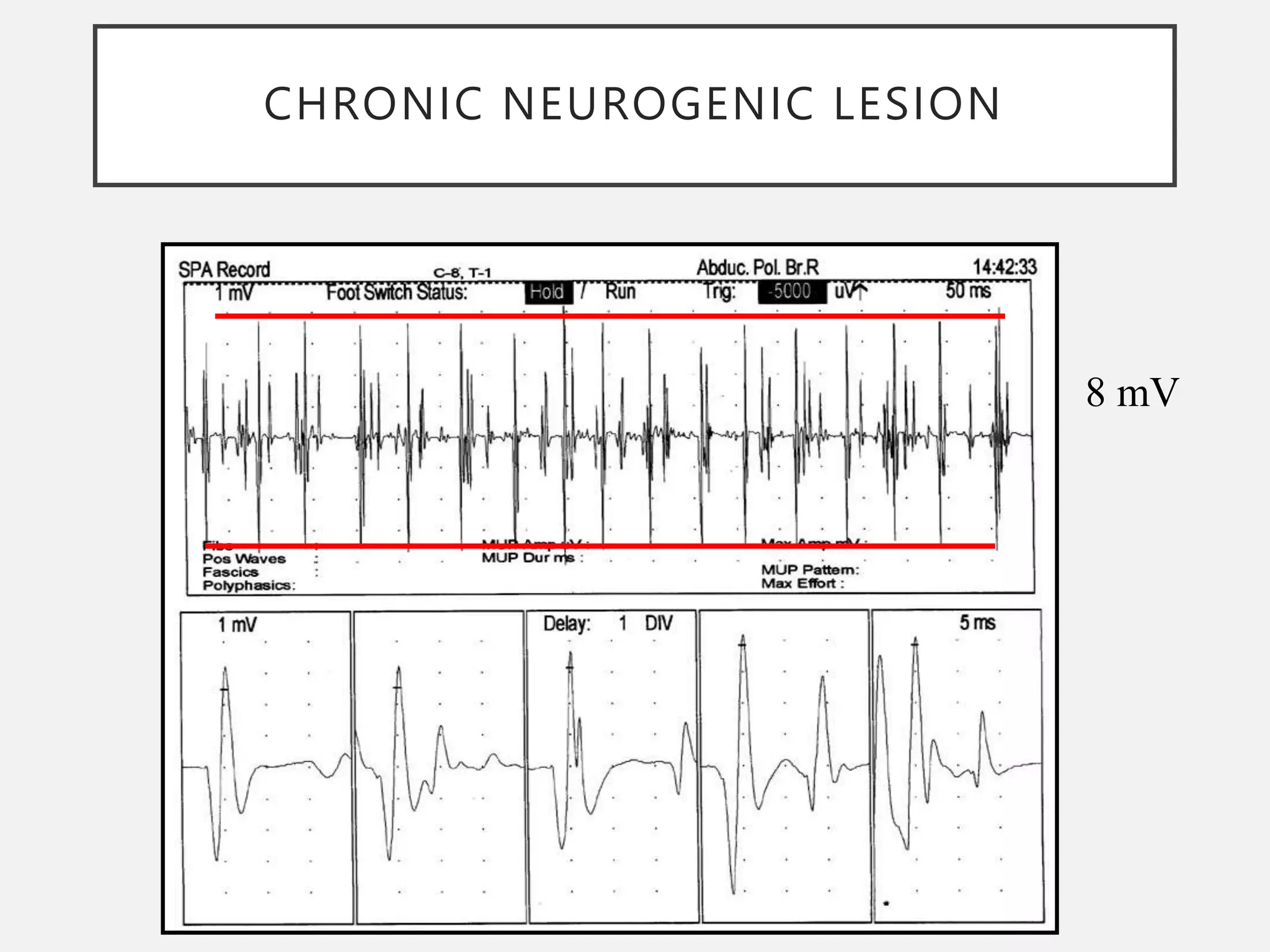
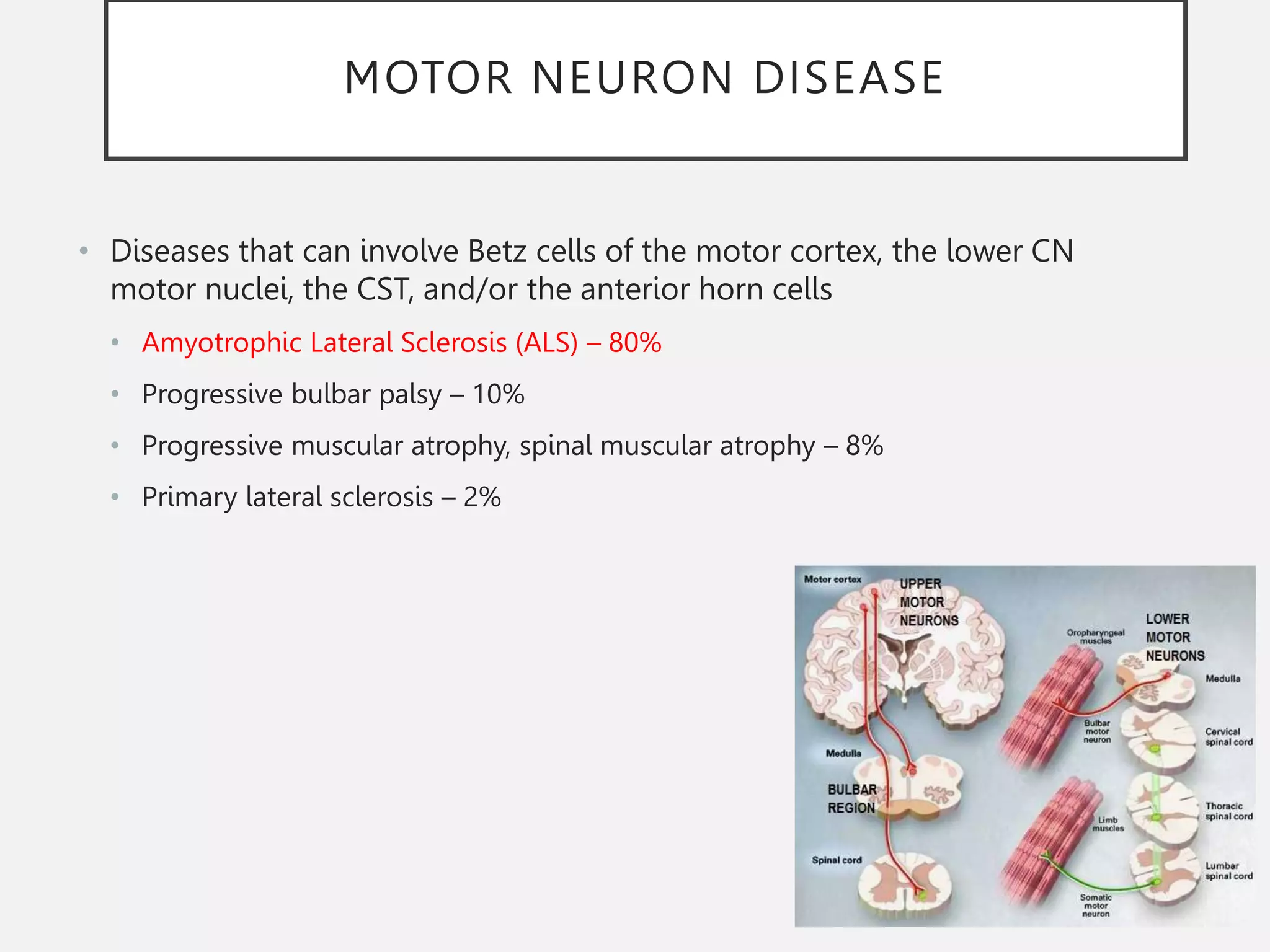
This document discusses neuromuscular diseases, focusing on peripheral nerve disorders, motor neuron disease, and myopathies. It describes various types of polyneuropathies including diabetic, chronic inflammatory demyelinating, and hereditary neuropathies. Guillain-Barré syndrome is discussed as an example of an acute polyneuropathy. Evaluation methods like electromyography and nerve conduction studies are also summarized.