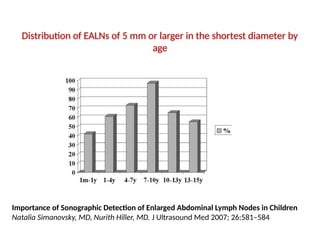
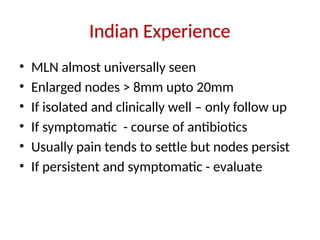
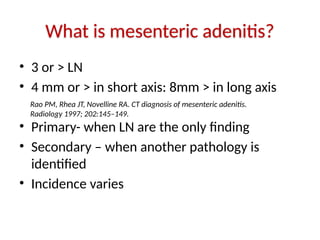
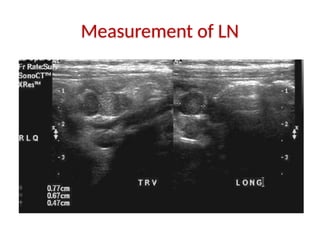
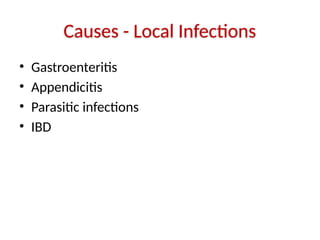
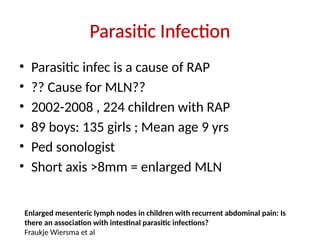
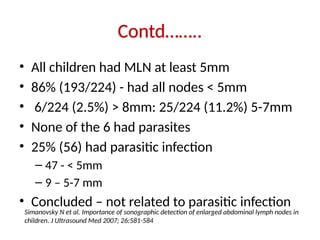
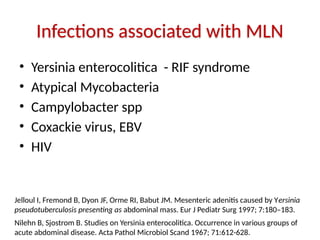
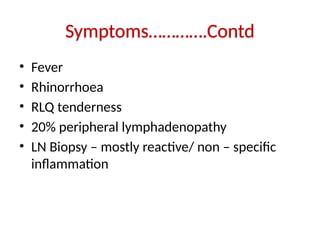
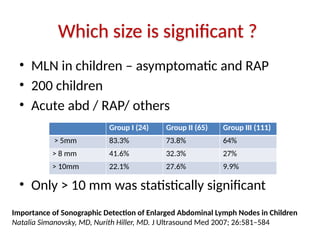
Mesenteric adenitis in children is often an incidental finding associated with recurrent abdominal pain and typically diagnosed via ultrasound, identifying mesenteric lymph nodes (MLN) that may indicate underlying infections or conditions. Studies suggest a low correlation between enlarged MLN and intestinal parasitic infections, and findings vary based on size and symptoms. Generally, if nodes are isolated and the child is asymptomatic, follow-up is recommended, while symptomatic cases may require treatment.




![Does Size Matter ?
• LN > 4mm seen in 4-64% asymp children
• 14-83% of symp children
• MLN are seen in all children – asymp, symp-
acute abd, CAP, gastroenteritis
• Tendency to have larger nodes in acute infect
• As an isolated finding – not much importance
Nan Fang Yi Ke Da Xue Xue Bao. 2011 Mar;31(3):522-4.
[Enlarged mesenteric lymph nodes in children: a clinical analysis with ultrasonography and the
implications].
[WANG WG, TIAN H, YAN JY, LI T, ZHANG TD, ZHAO YP, ZHANG LY, XING HG.
Sivit CJ, et al. Visualization of enlarged mesenteric lymph nodes at US examination. Pediatr Radiol
1993; 23:471-475
Rathaus Vet al Enlarged mesenteric lymph nodes in asymptomatic children: the value of the finding
in various imaging modalities. Br J Radiol 2005; 78:30-33](https://image.slidesharecdn.com/mesentericlapinchildren-241125070950-b5d3201e/85/Mesenteric-Lymphadenopathy-in-Children-ppt-16-320.jpg)