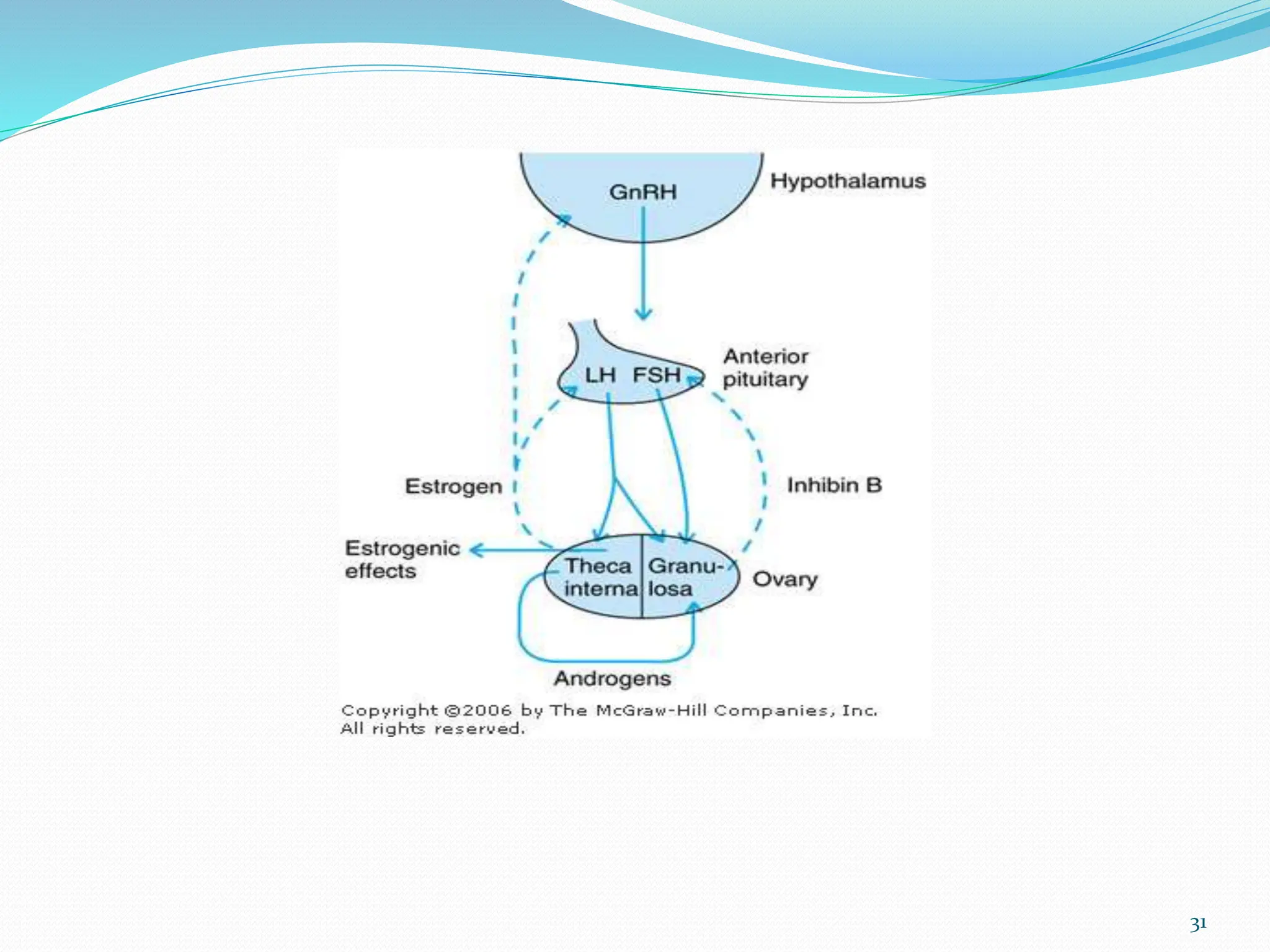
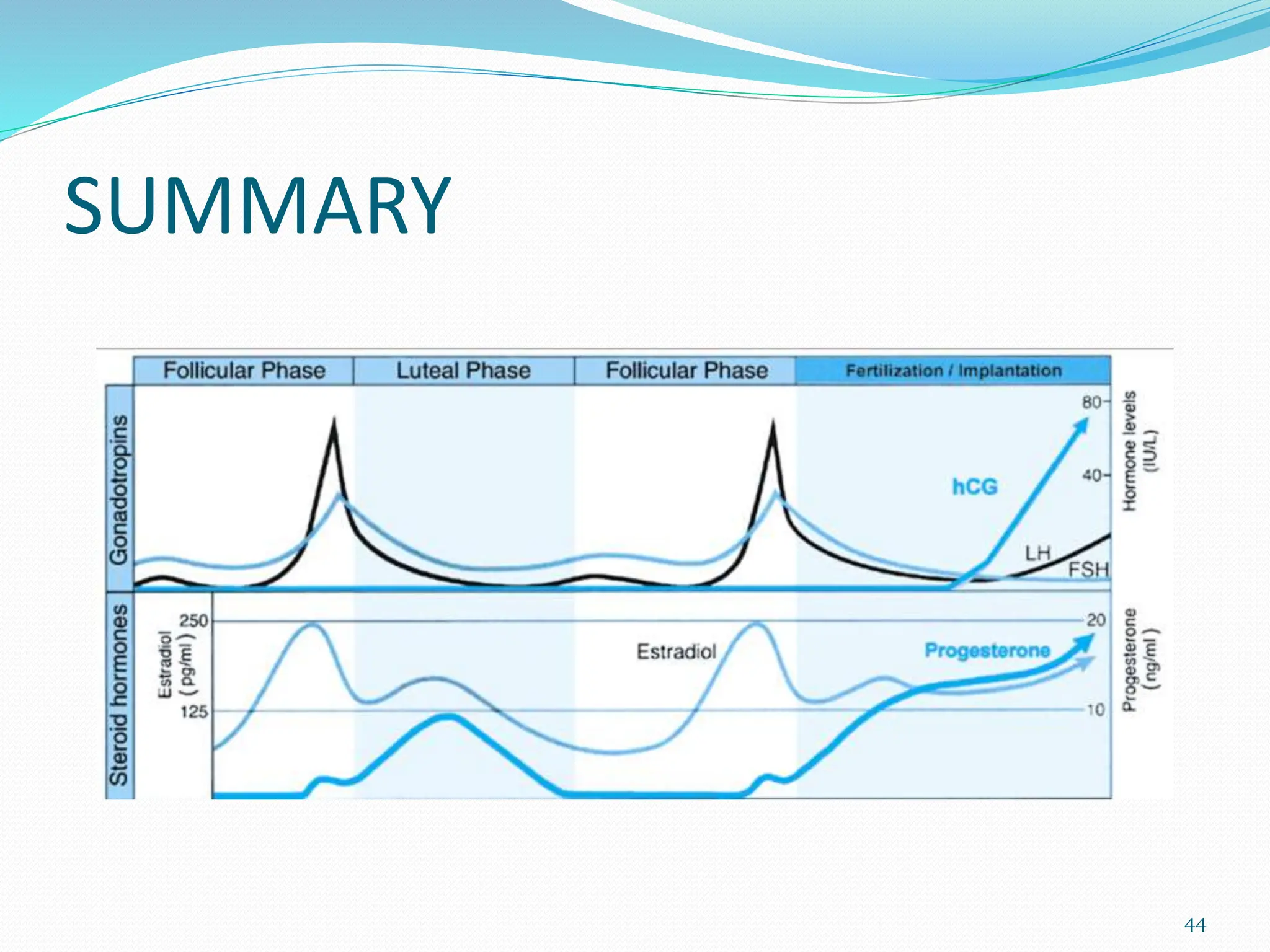
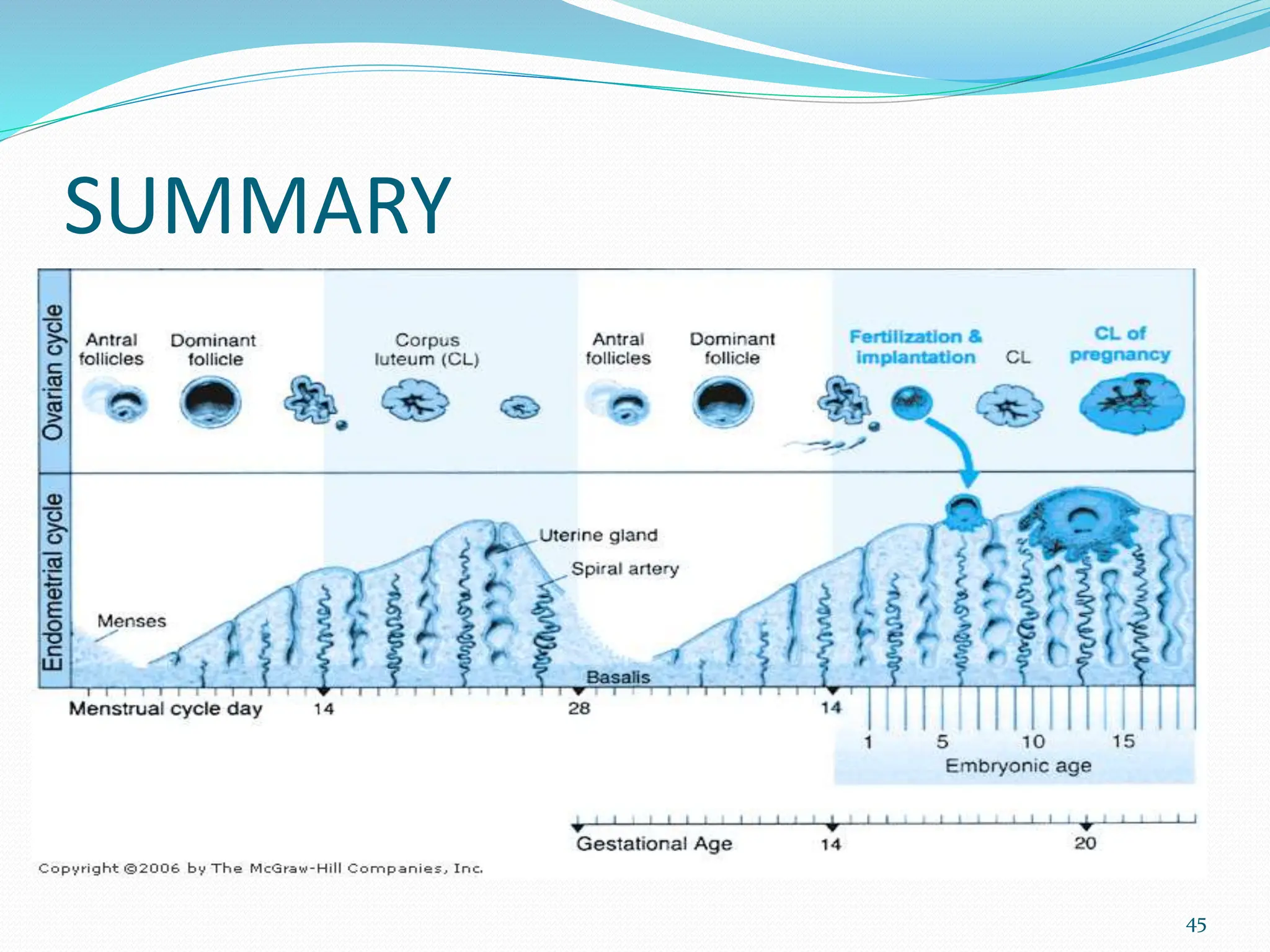
The menstrual cycle involves cyclic changes in the ovaries and uterus in preparation for potential pregnancy. The ovarian cycle occurs over approximately 28 days and includes follicular development, ovulation, and formation of the corpus luteum. The uterine cycle involves proliferation and secretory changes to the endometrium under the influence of ovarian hormones. Precisely coordinated fluctuations in hormones like estrogen, progesterone, FSH and LH regulate the menstrual cycle through negative feedback mechanisms.