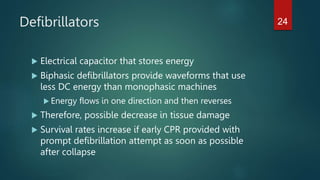
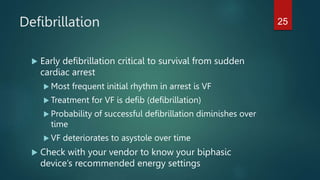
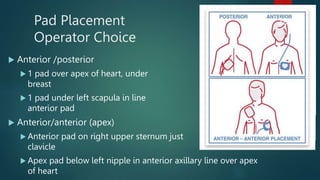
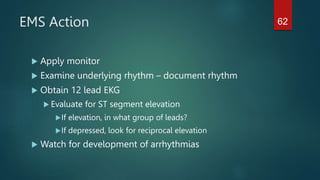
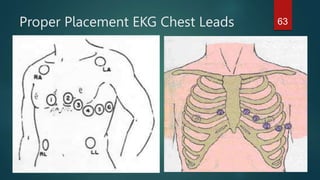
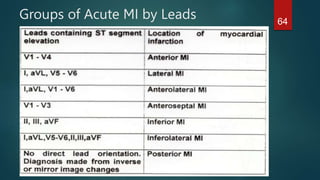
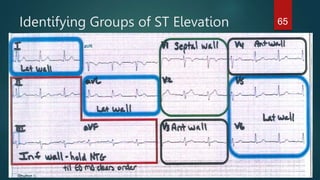
This document provides an overview of EMS equipment review objectives and topics. It will cover indications for various EMS equipment used in the field, managing equipment application, evaluating effectiveness, and participating in skills reviews. Specific equipment to be discussed includes capnography, defibrillators, endotracheal tubes, and pad placement for defibrillation. The goal is for participants to learn proper use and interpretation of this equipment to enhance patient care.