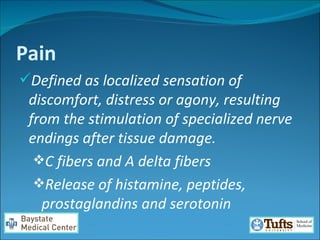
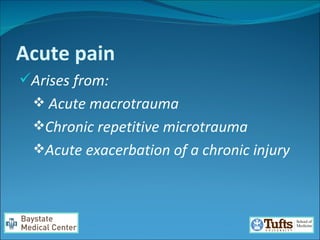
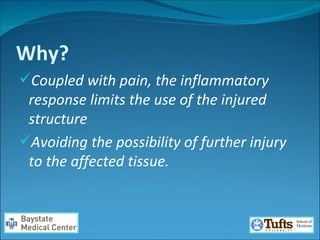
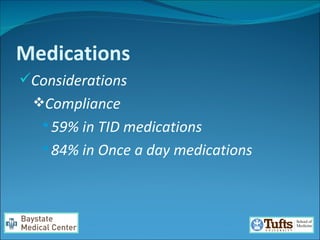
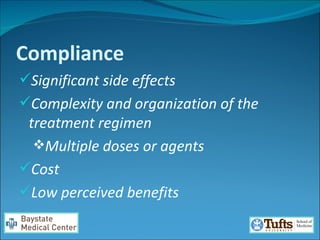
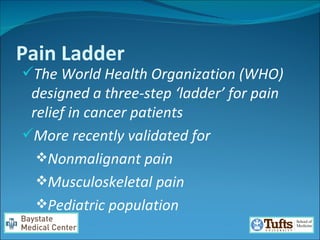
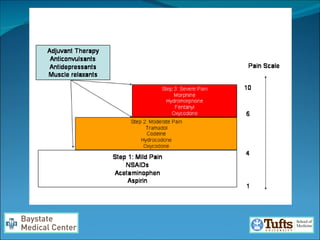
The document discusses management strategies for acute and subacute pain. It compares analgesic options and outlines the World Health Organization's three-step "pain ladder" approach. The pain ladder involves scheduled administration of medications ranging from non-steroidal anti-inflammatories to weak opioids like tramadol and strong opioids if needed. Proper use of analgesics requires considering factors like compliance, side effects, and risk of dependence.