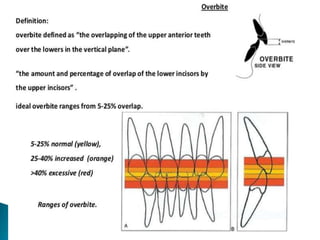
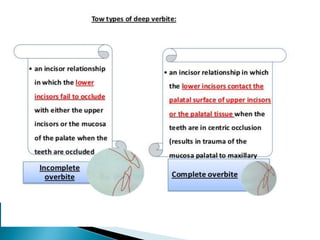
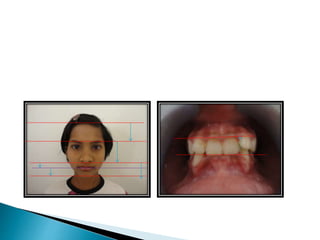
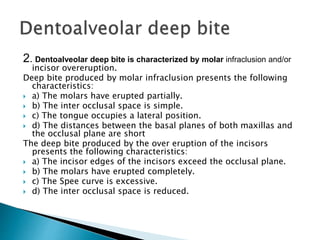
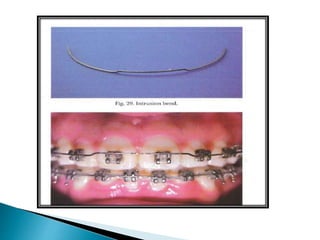
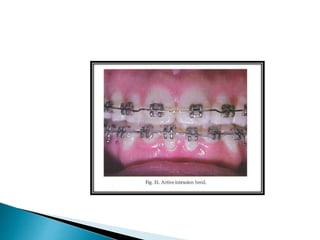
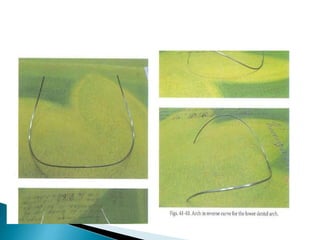
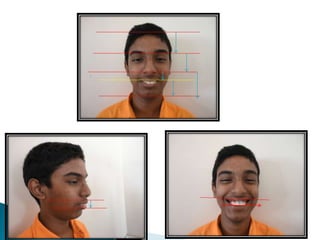
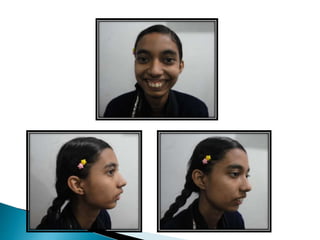
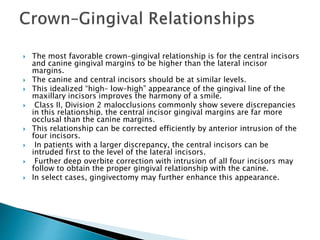
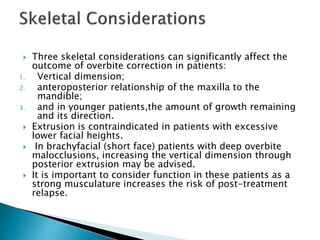
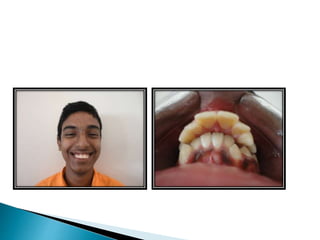
This document discusses types and treatment of deep bites. It describes skeletal vs dentoalveolar deep bites and factors that can cause acquired deep bites. The main treatment strategies discussed are extruding posterior teeth, flaring anterior teeth, and intruding incisors. Soft tissue considerations and their impact on treatment plan selection are also covered. Risks like apical root resorption from incisor intrusion are addressed.