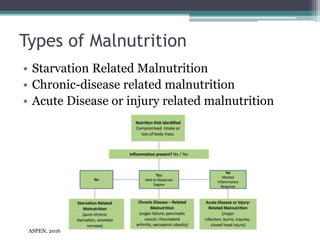
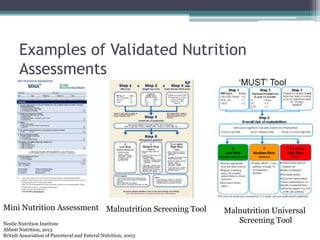
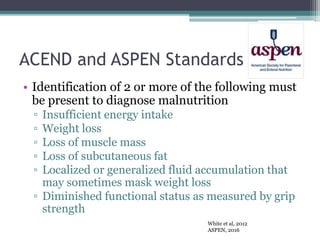
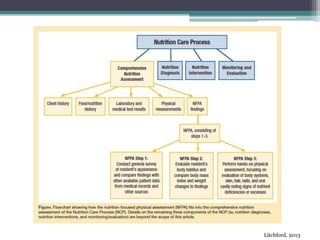
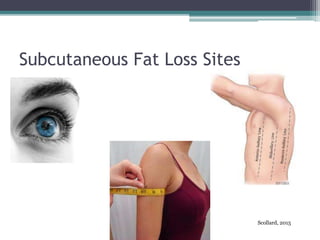
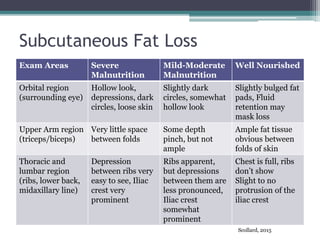
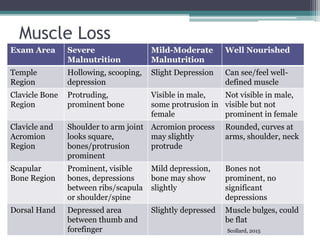
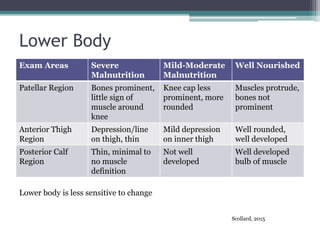
This document discusses malnutrition screening in acute care settings. It defines malnutrition and identifies risk factors such as acute or chronic illness. Causes of malnutrition include inadequate intake, impaired absorption, and social factors. The document reviews types of malnutrition and recommends screening tools to identify patients at risk. Signs of malnutrition include loss of muscle mass and subcutaneous fat. A nutrition-focused physical assessment is described to evaluate six body sites for muscle and fat loss. Complications of untreated malnutrition include increased mortality, longer hospital stays, and higher healthcare costs. Standardized screening tools are needed to properly identify and treat malnutrition.