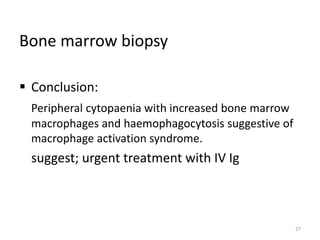
This document discusses the case of a 63-year-old woman with rheumatoid arthritis and diabetes who presented with chest pain and was diagnosed with a myocardial infarction. She subsequently developed fever and pancytopenia. Further tests found very high ferritin levels and a bone marrow biopsy confirmed macrophage activation syndrome, a severe complication caused by overly active immune cells. She was started on treatment including steroids and IVIG but unfortunately died shortly after being transferred to the ICU. The key lessons are that macrophage activation syndrome can occur in adults with autoimmune conditions and be fatal if not recognized and treated promptly.










![ ESR – 133 mm 1st h
CRP – 129 mg/dl
UFR – RBC field full
S.cr – 3.24 mg/dl
Clotting profile
APTT – 35 sec.
INR - 1
Serum Ferritin – 1196 ng/ml [20 – 400 ng/l]
13](https://image.slidesharecdn.com/macrophageactivation-170312165129/85/Macrophage-activation-13-320.jpg)

![ Problem list.
In a patient with sero negative RA, on Methotrexate
Recent, STEMI
Mild Fever with Pancytopaenia
Gum bleeding with normal clotting profile [low platelet].
Multiple small joint pain, swelling, with minimal morning stiffness with
high inflammatory markers.
Deranged liver function, marginally low albumin, predominantly
cholestatic
Renal impairment (Acute kidney injury)
15](https://image.slidesharecdn.com/macrophageactivation-170312165129/85/Macrophage-activation-15-320.jpg)