This document discusses lumbar motor control training for chronic low back pain. It begins by reviewing evidence that motor control exercises are effective at improving pain and function compared to minimal interventions. The goal of motor control training is to retrain core muscles like transversus abdominis to maintain low-level contractions during daily activities. Initial training focuses on precise isolation of these muscles in non-weight bearing positions before progressing to functional exercises. Various techniques are described to facilitate muscle activation, including use of verbal and tactile cues and different body positions. Proper dosage and development of kinesthetic awareness are also emphasized to transfer skills to functional tasks.
![Introduction
• Motor control exercise is a popular form
of exercise that aims to restore co-
ordinated and efficient use of the muscles that
control and support the spine. The therapist
guides the client to practise normal use of the
muscles during simple tasks. As control and
skill improve the exercises are progressed to
more complex and functional tasks involving
the muscles of the trunk and limbs[1].](https://image.slidesharecdn.com/lumbarmotorcontroltraining-221124054217-01b3af1c/85/Lumbar-Motor-Control-Training-pptx-2-320.jpg)
![• A 2016 systematic review evaluating the effectiveness of motor
control exercise (MCE) in patients with chronic non-specific low
back pain concluded:
• "MCE probably provides better improvements in pain, function and
global impression of recovery than minimal intervention at all
follow-up periods. MCE may provide slightly better improvements
than exercise and electrophysical agents for pain, disability, global
impression of recovery and the physical component of quality of
life in the short and intermediate term. There is probably little or no
difference between MCE and manual therapy for all outcomes and
follow-up periods. Little or no difference is observed between MCE
and other forms of exercise. Given the minimal evidence that MCE
is superior to other forms of exercise, the choice of exercise for
chronic LBP should probably depend on patient or therapist
preferences, therapist training, costs and safety".[1]](https://image.slidesharecdn.com/lumbarmotorcontroltraining-221124054217-01b3af1c/85/Lumbar-Motor-Control-Training-pptx-3-320.jpg)
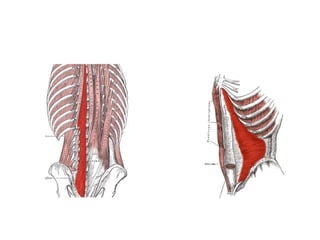
![• The goal of the motor control program is to
retrain the core muscles of the lumbar spine,
comprising transversus abdominis,
lumbar multifidus and the pelvic floor, to
maintain a tonic and automatic
contraction[21][47] at less than 30% of
maximum voluntary contraction in daily
activities[31][29].](https://image.slidesharecdn.com/lumbarmotorcontroltraining-221124054217-01b3af1c/85/Lumbar-Motor-Control-Training-pptx-5-320.jpg)

![• In most cases this requires initial training in non-weight bearing positions using a
lower abdominal drawing in manoeuvre which has been shown to selectively
activate transversus abdominis.[23] Lumbar multifidus and the pelvic floor muscles,
including pubococcygeus, have been shown to co-contract with transversus
abdominis to provide a “corset” for the lumbo-pelvic area[48][49] and practitioners
should aim to achieve such a result in association with the lower abdominal
drawing in manoeuvre.
• Training should initially focus on quality of movement and precise isolation of the
relevant core muscles which has been shown to be important in restoring normal
motor control in people with LBD.[29][31]
• Once adequate motor control of the core muscles is achieved in non-weight
bearing positions, subsequent progression to functional activities can be
made.[3][23] Importantly this progression involves integration of the global muscles
of the spine with the core muscles during specific functional exercises as well as
during strength training of the trunk.[36]
• There is emerging evidence that functional retraining of normal lumbo-pelvic
kinematics can improve motor control and clinical outcomes[50] and these methods
should also be considered during functional motor control exercises.](https://image.slidesharecdn.com/lumbarmotorcontroltraining-221124054217-01b3af1c/85/Lumbar-Motor-Control-Training-pptx-7-320.jpg)
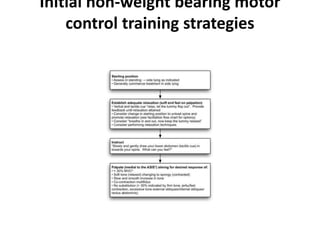
![• Adequate relaxation of the global muscles, eg rectus abdominis, external obliques
and erector spinae, is required before attempting to contract the core stability
muscles. Patients with maladaptive motor control strategies commonly
demonstrate a dominance of the global muscles during functional tasks and at
rest.[13][47] In retraining a normal motor control pattern, adequate relaxation is an
important first step in inhibiting tone of the global muscles, thereby allowing a
more isolated contraction of the core muscles.[51] In attaining a relaxed state, a
neutral spine position should also be encouraged, as this appears to improve
activation of the core muscles.[3][52]
• An instruction to “draw the lower abdomen in towards the spine” should be used
consistent with the developers of the abdominal drawing in method.[3]
• In addition to these standard instructions, the terms “slowly” and “gently” can be
added to emphasise the sub-maximal nature of the contraction.[53]
• Tactile cues to the lower abdomen should be used in conjunction with verbal cues
to provide additional emphasis on a lower rather than more general drawing in of
the abdomen.[3]
• Non-weight bearing positions should be selected in the position where best
activation of transversus abdominis is observed,[3][54] however side lying is
commonly the optimal position for initial retraining[55] due to ease of obtaining
relaxation of the global muscles and an improved length tension relationship in
transversus abdominis compared to other positions (eg supine or crook lying).](https://image.slidesharecdn.com/lumbarmotorcontroltraining-221124054217-01b3af1c/85/Lumbar-Motor-Control-Training-pptx-9-320.jpg)
![• Palpation
• Primary outcomes indicative of an adequate and sub-maximal transversus
abdominis contraction are a 2-3cm isolated inward movement of the
abdomen approximately 3cm above the pubic symphysis and a palpable
slow and co-ordinated change in tone from a “soft” feel in the relaxed
state to a “spongy” feel at sub-maximal contraction.[53]
• These palpatory findings provide the physiotherapist with information
additional to observation regarding the sub-maximal nature of the
contraction.[53]
• The physiotherapist can concurrently palpate adjacent to the L3-L5
spinous processes to assess for co-contraction of lumbar multifidus, in the
process identifying whether specific multifidus retraining is also required
to achieve normal motor control. Well documented substitution
strategies[3] should be monitored, and patient feedback provided, to
ensure the observed drawing in of the lower abdomen and the palpatory
findings are not the result of activity from the global muscles, in particular
internal obliques.](https://image.slidesharecdn.com/lumbarmotorcontroltraining-221124054217-01b3af1c/85/Lumbar-Motor-Control-Training-pptx-10-320.jpg)

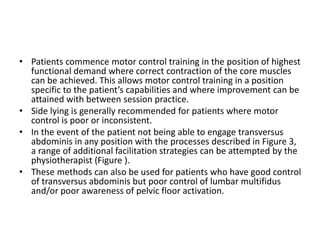
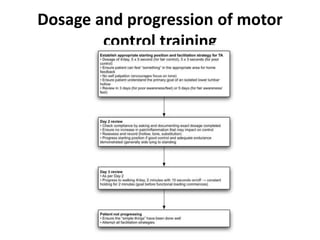
![• In patients where transversus abdominis is difficult to isolate, activation was facilitated by an initial
focus on the pelvic floor and/or lumbar multifidus.[3][56] In such cases the strategies listed in Figure
6 are applied and co-contraction of transversus abdominis is concurrently monitored. In the event
of co-contraction occurring, the patient should be encouraged to focus on awareness of
simultaneous activation of transversus abdominis as well as the pelvic floor and/or lumbar
multifidus. The pelvic floor instructions aim to illustrate the anatomy of the region and provide
guidance in performing a submaximal isotonic contraction. The multifidus instructions aim to
provide guidance in performing a submaximal isometric contraction. If necessary, multifidus can be
facilitated by provision of kinaesthetic feedback to the patient with an initial isotonic contraction,
followed by an attempt to transfer this awareness to the required isometric contraction.
• During all motor control training the patient should be encouraged to develop a kinaesthetic
awareness of the correct motor pattern. This is important in order for the patient to have some
form of proprioceptive feedback regarding correct performance of the exercises when practising
between sessions.[3] Subsequently during the treatment program, adequate kinaesthetic awareness
of normal motor control is also required for transference into more functional and demanding
exercises/activities. Due to the effect of even low force postural perturbation in initiating
maladaptive motor patterns,[19][20][22] patients should be instructed not to self palpate as means of
providing feedback on exercise performance until more consistent motor control skills are
demonstrated. Self palpation can also focus the patient on tone rather than the primary goal of an
isolated drawing in of the lower abdomen.
• Once an appropriate motor control strategy, exercise and starting position has been identified, a
detailed information sheet should be provided and explained to the patient. The content should
include information on the anatomy and normal function of the core muscles, the general principle
of progressing motor control training from non-weight bearing to functional activities, and
instructions for between session practice. The physiotherapist should document an appropriate
dosage regime on the information sheet according to the principles outlined in Figure 6. Over the
following sessions the physiotherapist, working with the patient, should aim to achieve a tonic
contraction of the core muscles, during walking for two minutes before progressing to more
advanced functional training.](https://image.slidesharecdn.com/lumbarmotorcontroltraining-221124054217-01b3af1c/85/Lumbar-Motor-Control-Training-pptx-14-320.jpg)