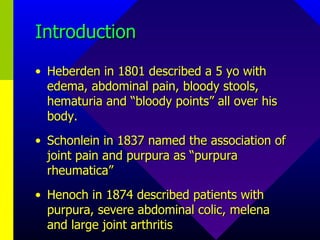
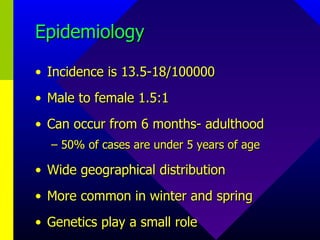
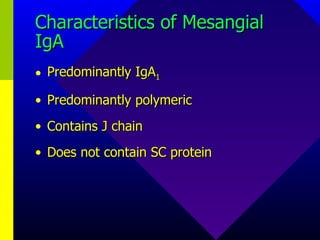
Henoch-Schonlein Purpura (HSP) is the most common vasculitis in children that causes a rash, joint pain, abdominal pain, and kidney inflammation. It is considered a type of IgA nephropathy with extrarenal symptoms. HSP typically affects young children and has a classic presentation of purpura rash, abdominal pain, and arthritis. It can involve the skin, joints, gastrointestinal tract, and kidneys. Treatment focuses on managing symptoms, with steroids sometimes used for severe or persistent cases to help prevent long-term kidney damage.