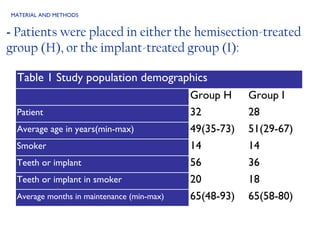
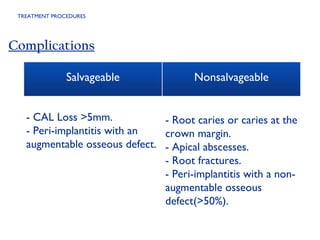
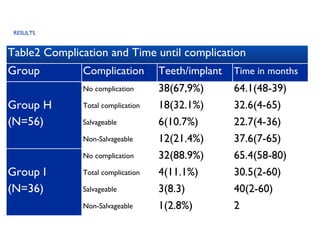
This retrospective study compares the long-term complication and survival rates of root-resected mandibular molars and dental implants in patients with grade III furcation involvement. Results indicate that while both treatments can achieve approximately six years of complication-free survival, root-resected molars exhibit a higher risk for complications. The study suggests that dental implants replacing periodontally involved molars result in fewer complications than hemisected molars, although further research is required for generalization.