1) Communities play a central role in health promotion through social ties and networks that influence health. However, persistent health inequalities remain a challenge.
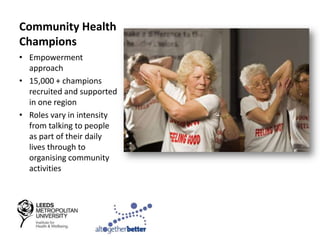
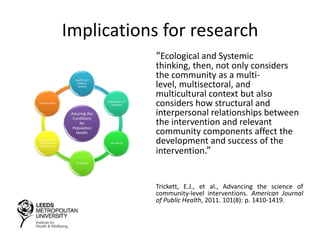
2) Community-based interventions show promise but it is unclear if their local impacts can address population-level inequalities. Developing an evidence base to support this work is important.
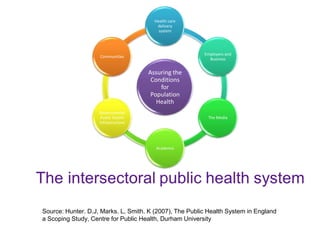
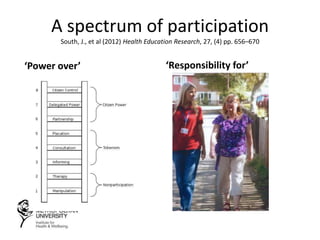
3) Effective community participation in health policy and implementation requires designing health systems that facilitate involvement and connect community voices to decision-making.