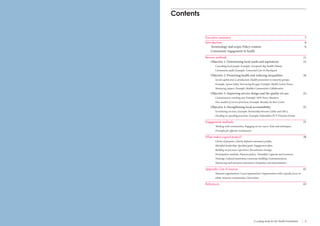
This document discusses community engagement for health improvement. It identifies four key roles for community engagement: 1) determining local needs and aspirations, 2) promoting health and reducing inequalities, 3) improving service design and quality of care, and 4) strengthening local accountability. The document reviews different approaches to community engagement in the UK, presents examples of relevant initiatives, and identifies characteristics of successful community engagement projects, including clarity of purpose, leadership, engagement strategies, and evaluation. The goal is to inform the Health Foundation's efforts to strengthen community engagement in health.