This document outlines the steps for investigating an epidemic:
1) Verify diagnoses of cases and confirm the epidemic exceeds expected occurrences.
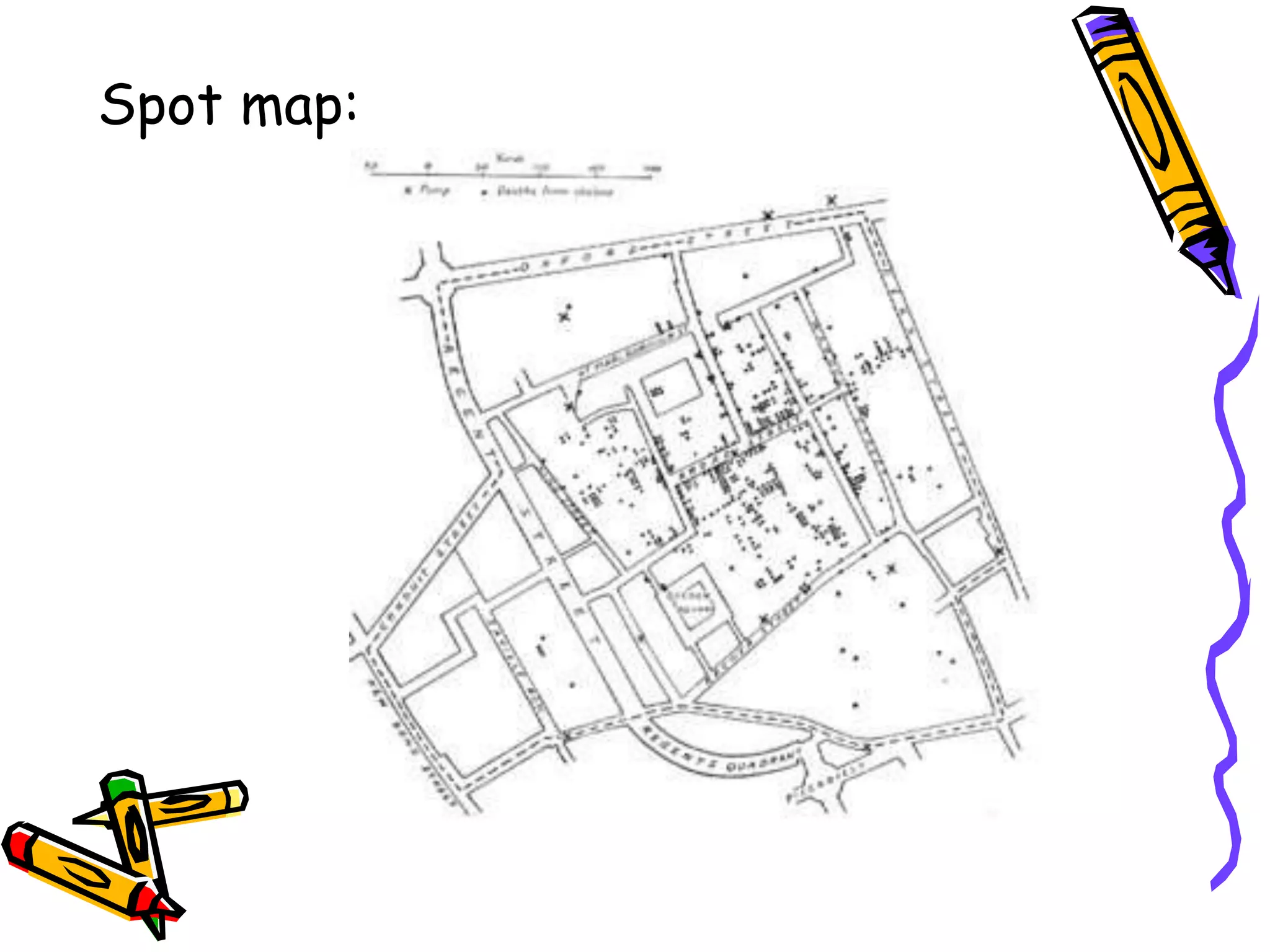
2) Define the at-risk population by mapping the area and counting residents.
3) Rapidly identify all cases through medical surveys and ask cases about other potential cases.
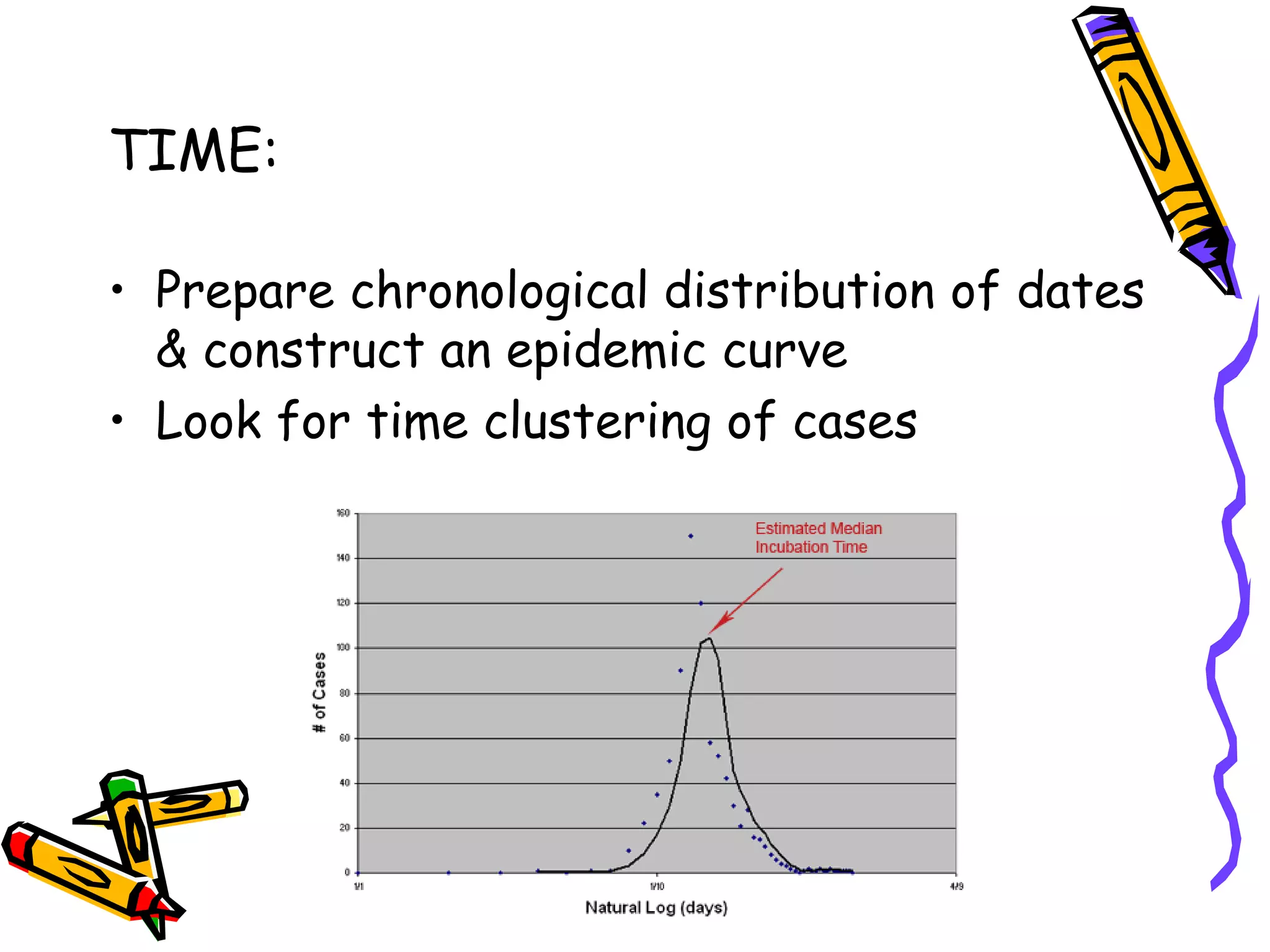
4) Analyze collected data on time, place, and person to identify common factors and form a hypothesis about the source and transmission of the disease.