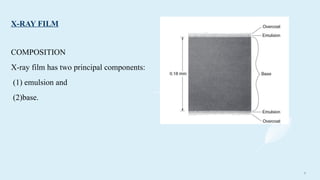
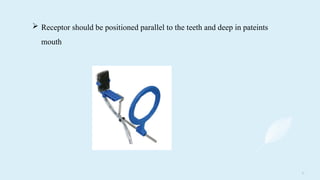
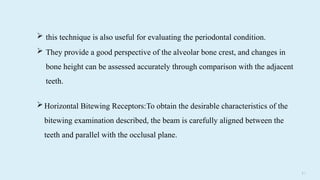
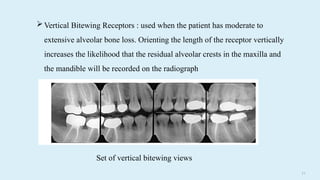
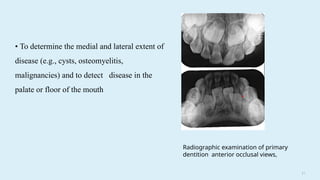
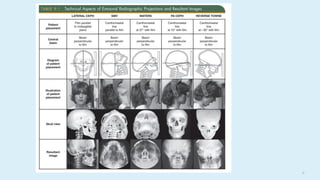
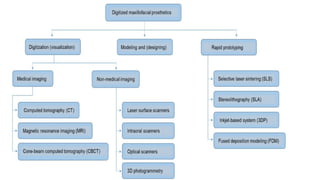
The document outlines various imaging techniques used in dentistry, emphasizing the importance of dental radiographs for diagnosing conditions not visible clinically. It details different types of radiographs (intraoral and extraoral), techniques for obtaining images, and the technologies involved, including digital imaging and cone-beam computed tomography. The document also highlights the applications of various imaging techniques in treatments and evaluations related to dental health and prosthodontics.