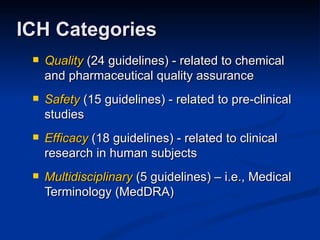
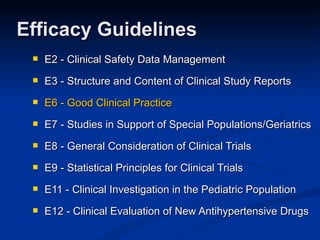
- The document compares the FDA regulations for clinical trials to the International Conference on Harmonization's (ICH) Good Clinical Practice (GCP) guidelines.
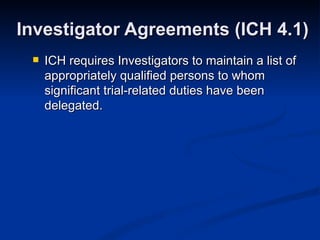
- There are some differences between the two, such as ICH requiring more documentation of trial procedures and delegation of duties, while FDA regulations are less specific.
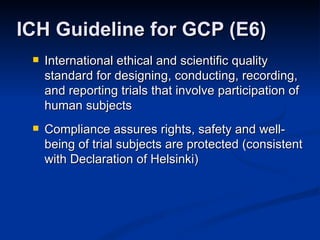
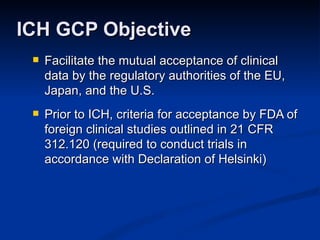
- Overall ICH GCP guidelines facilitate international harmonization and acceptance of clinical trial data between the US, EU, and Japan. Compliance with ICH GCP helps assure rights and safety of trial subjects.




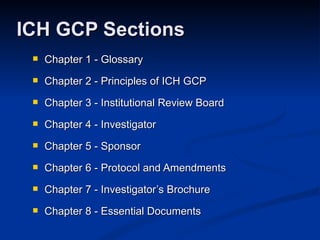
![ICH has more detailed outline of contents of the protocol and Investigator Brochure than the FDA regulations [21 CFR 312.23(a)(5-6)] ICH requires that the protocol identify any data to be recorded directly on the CRFs and to be considered source data (ICH 6.4.9) Protocol and IB (ICH 6 & 7)](https://image.slidesharecdn.com/ichfdasocra092007-1227183704282746-9/85/Ich-Fda-Socra-09-2007-38-320.jpg)

![Office: (952) 882-4083 E-mail: [email_address] Contact Information](https://image.slidesharecdn.com/ichfdasocra092007-1227183704282746-9/85/Ich-Fda-Socra-09-2007-42-320.jpg)