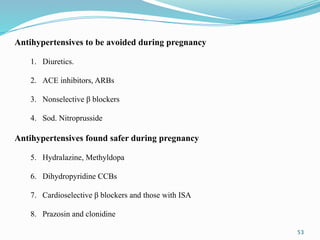
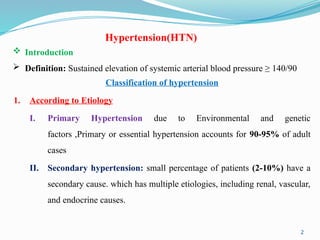
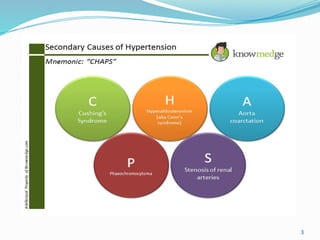
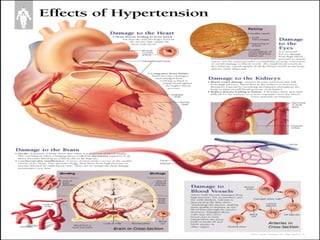
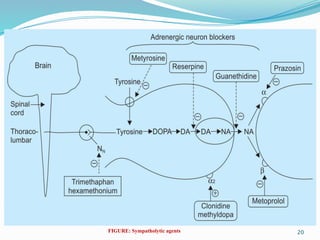
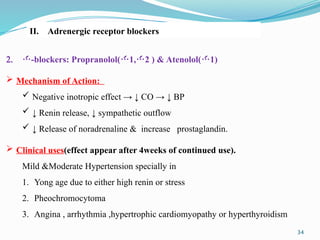
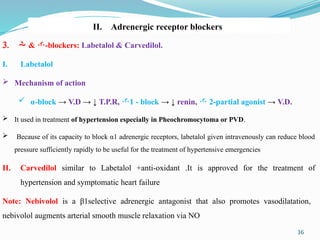
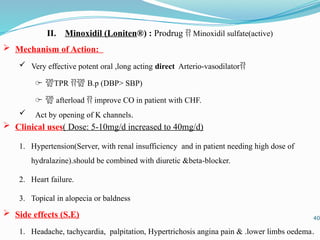
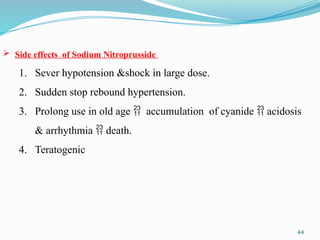
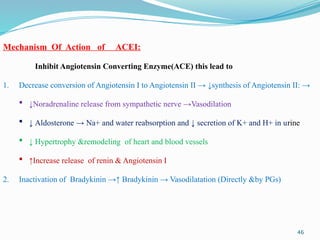
The document provides an overview of hypertension, including its definitions, classifications, and physiological principles for blood pressure regulation. It discusses the etiology of hypertension, treatment options that encompass lifestyle changes and pharmacotherapy, detailing various anti-hypertensive drug classes and their mechanisms of action. Additionally, the document outlines the side effects and clinical uses of specific medications, emphasizing the importance of tailored treatment strategies for managing hypertension.




































![52
3) Direct Renin Inhibitor: Aliskiren
1. newest agent, introduced 2005, Expensive.
2. direct renin inhibitor → production of angiotensin I
3. actions similar to ACEI but not associated with dry cough (no bradykinin)
4. less likely to cause angioedema, glossitis, oral ulceration, rash
5. adverse effects and contraindications similar to ACEIs/ARBs
6. used if cannot tolerate ACEIs or ARBs
7. poor bioavailability < 5%, may [furosemide] (MOA unknown)
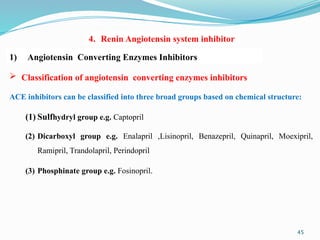
4. Renin Angiotensin system inhibitor](https://image.slidesharecdn.com/hypertensionlecture-5-240912165238-c1f26194/85/Hypertension-Lecture-5-pptx-for-pharmacy-students-52-320.jpg)