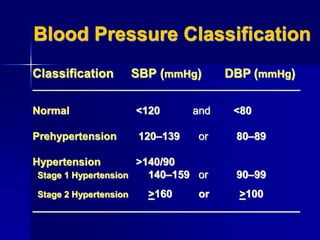
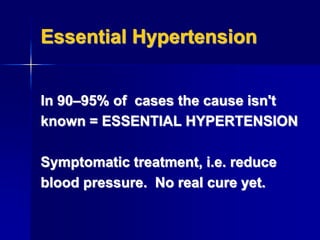
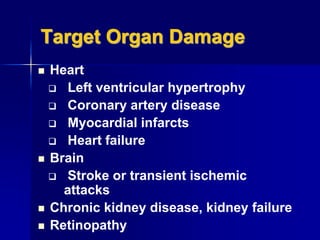
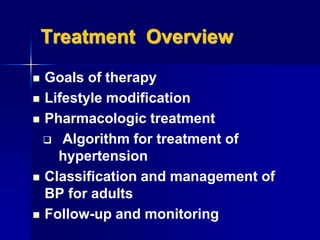
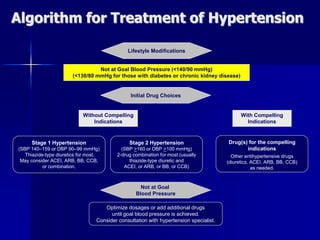
The document discusses various aspects of antihypertensive agents, detailing blood pressure classifications and the prevalence of hypertension. It outlines treatment approaches including lifestyle modifications and pharmacological options, emphasizing the importance of diuretics and other drug classes like ACE inhibitors and vasodilators. The document also highlights the significance of monitoring and managing complications associated with hypertension.