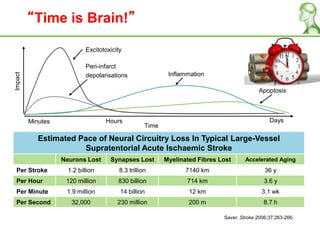
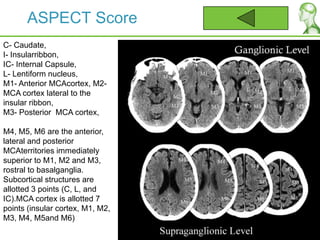
1. The document discusses guidelines and initiatives for treating acute ischemic stroke, including the importance of rapid treatment to minimize brain damage.
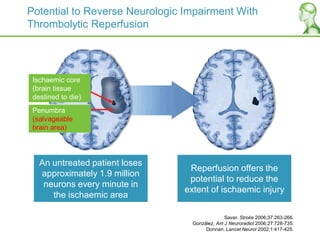
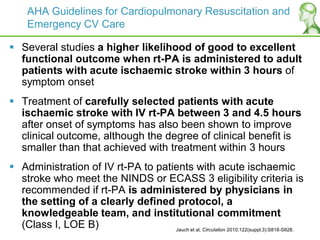
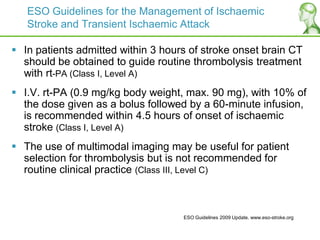
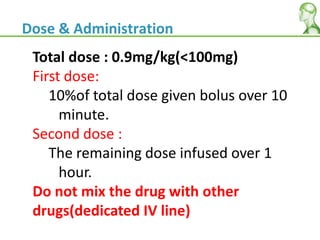
2. It describes the Hospital Kuala Lumpur Acute Ischemic Stroke Thrombolysis Initiatives (HASTE), which takes a multidisciplinary approach to treat stroke patients within 3 hours of onset to potentially reverse neurological impairment through thrombolytic reperfusion.
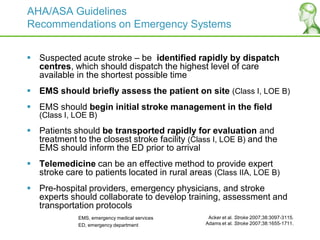
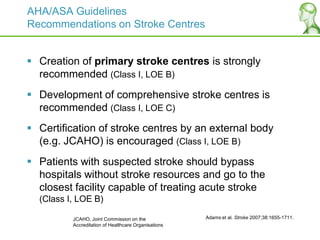
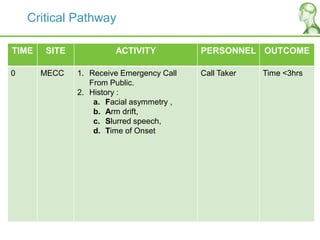
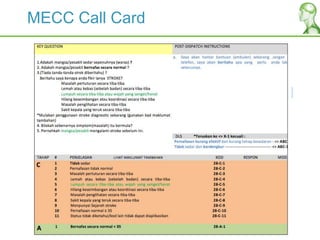
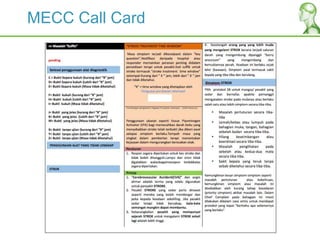
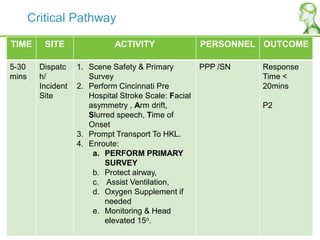
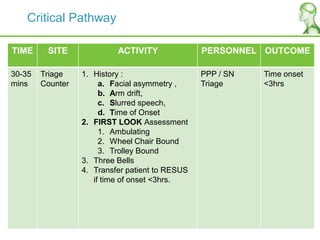
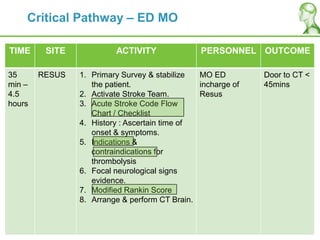
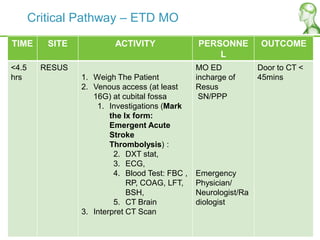
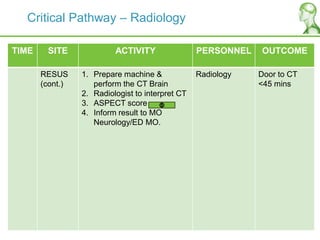
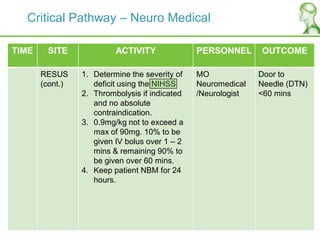
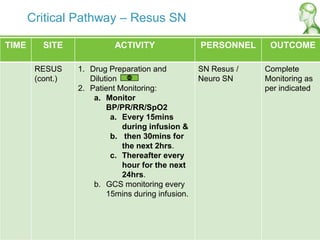
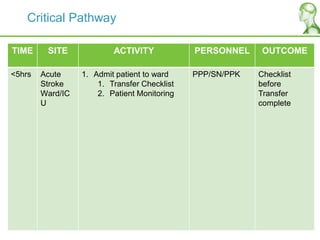
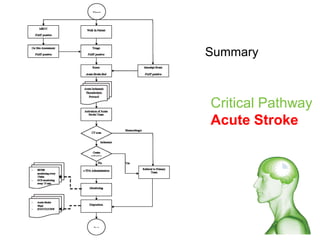
3. The HASTE program developed a critical pathway to rapidly identify, assess, and treat potential stroke patients from the emergency call through transport, the emergency department, and thrombolysis treatment.