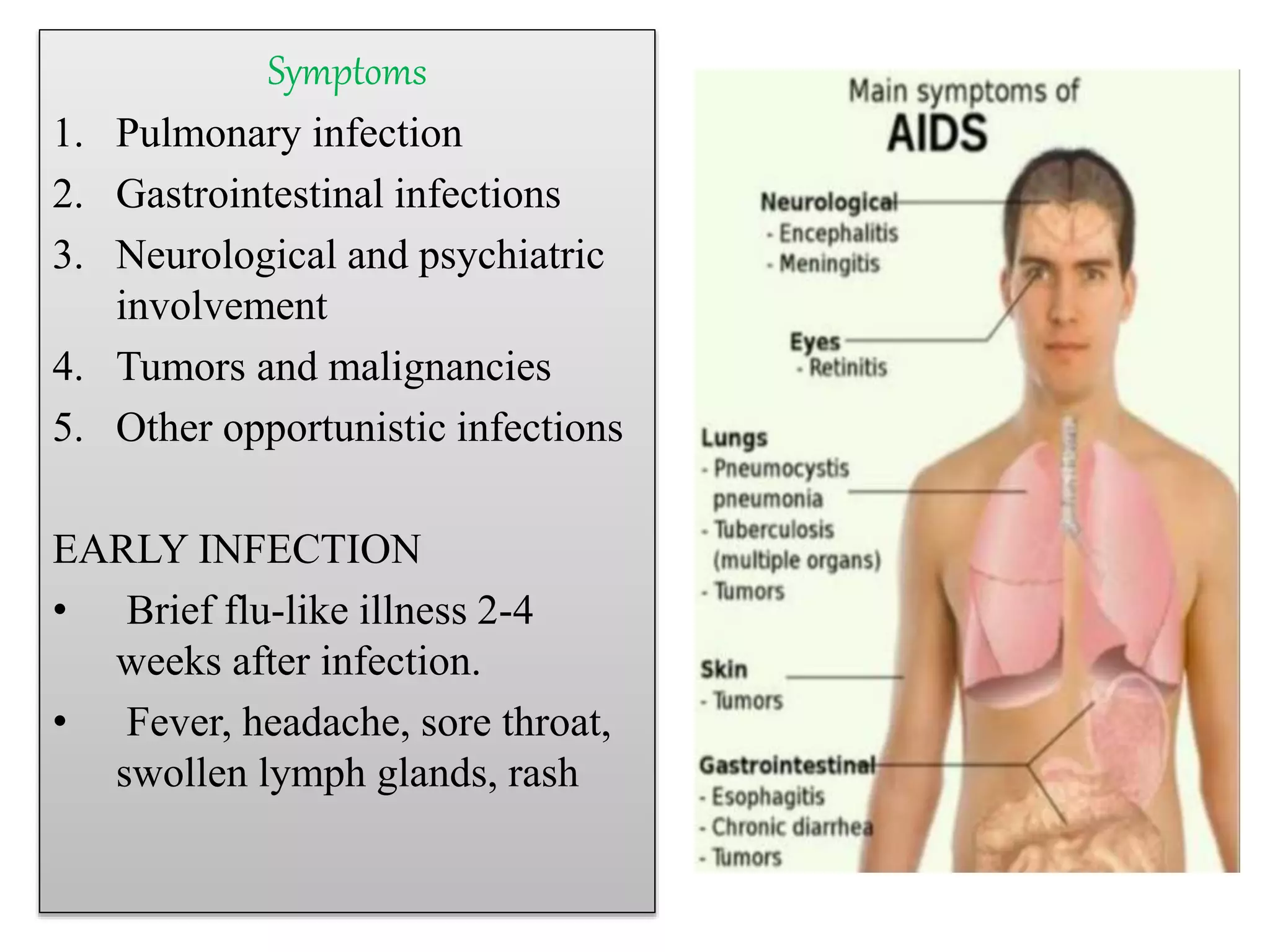
HIV is a retrovirus that infects and destroys CD4+ T cells, weakening the immune system and allowing opportunistic infections. Opportunistic infections are uncommon infections that take advantage of a weakened immune system. The stages of HIV are primary infection, asymptomatic, symptomatic, and AIDS. Treatment involves antiretroviral therapy to suppress the virus along with treatment of opportunistic infections. Care must also be taken with co-infections like hepatitis and malignancies associated with AIDS.

![HIV (Human
immunodeficiency virus)
• RNA retrovirus of the
genes lentivirus that infects
and destroys viral cells of
the human immune system,
such as helper T cells.
[CD4+ cells]
•HIV-1 : most common.
•HIV-2 :limited to West
Africa.
•It causes AIDS](https://image.slidesharecdn.com/hivandopportunisticinfection-sowparnika-200514084658/75/Hiv-and-opportunistic-infection-2-2048.jpg)