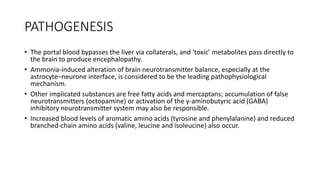
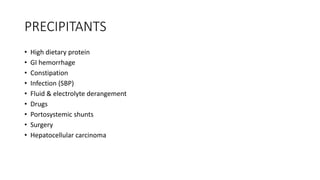
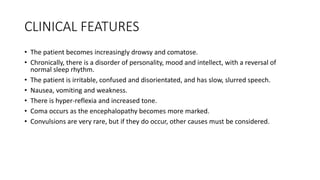
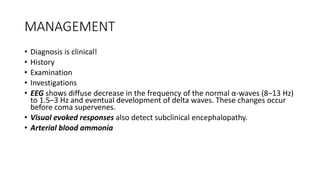
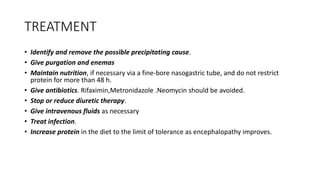
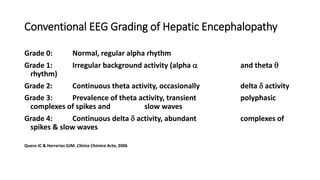
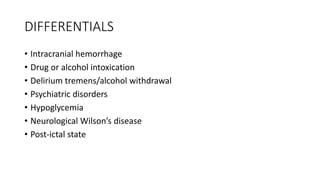
Hepatic encephalopathy is a neuropsychiatric syndrome that occurs secondary to liver disease and portosystemic shunting. It is caused by toxic metabolites like ammonia that bypass the liver and affect the brain. Clinical features range from subtle personality changes to confusion, coma, and death in acute liver failure. Treatment involves identifying and removing precipitants, providing nutrition support, antibiotics, and procedures to reduce ammonia levels like lactulose. Prognosis depends on the underlying liver disease severity.