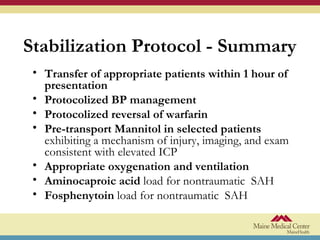
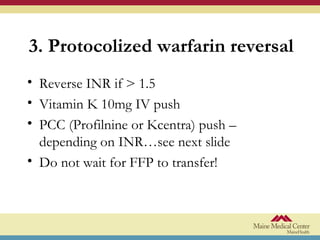
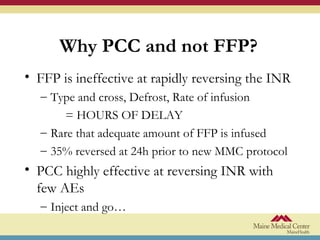
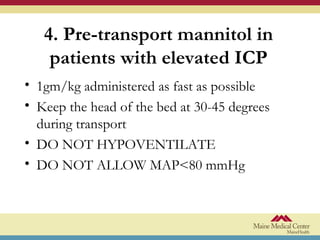
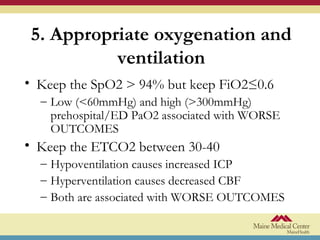
This document presents a stabilization protocol for patients with hemorrhagic stroke during pre-hospital transport and upon arrival at the hospital. The goals are to prevent clinical decline and improve outcomes by protocolizing blood pressure management, warfarin reversal, use of mannitol for elevated intracranial pressure, appropriate oxygenation and ventilation, administration of antifibrinolytic and anti-seizure medications, and ensuring ultra-early transfer to a specialized stroke center. Key elements include transferring patients within 1 hour, maintaining systolic blood pressure below 140 mmHg, rapidly reversing elevated INR, administering mannitol or medications pre-transport if indicated, and monitoring for protocol adherence and patient outcomes.