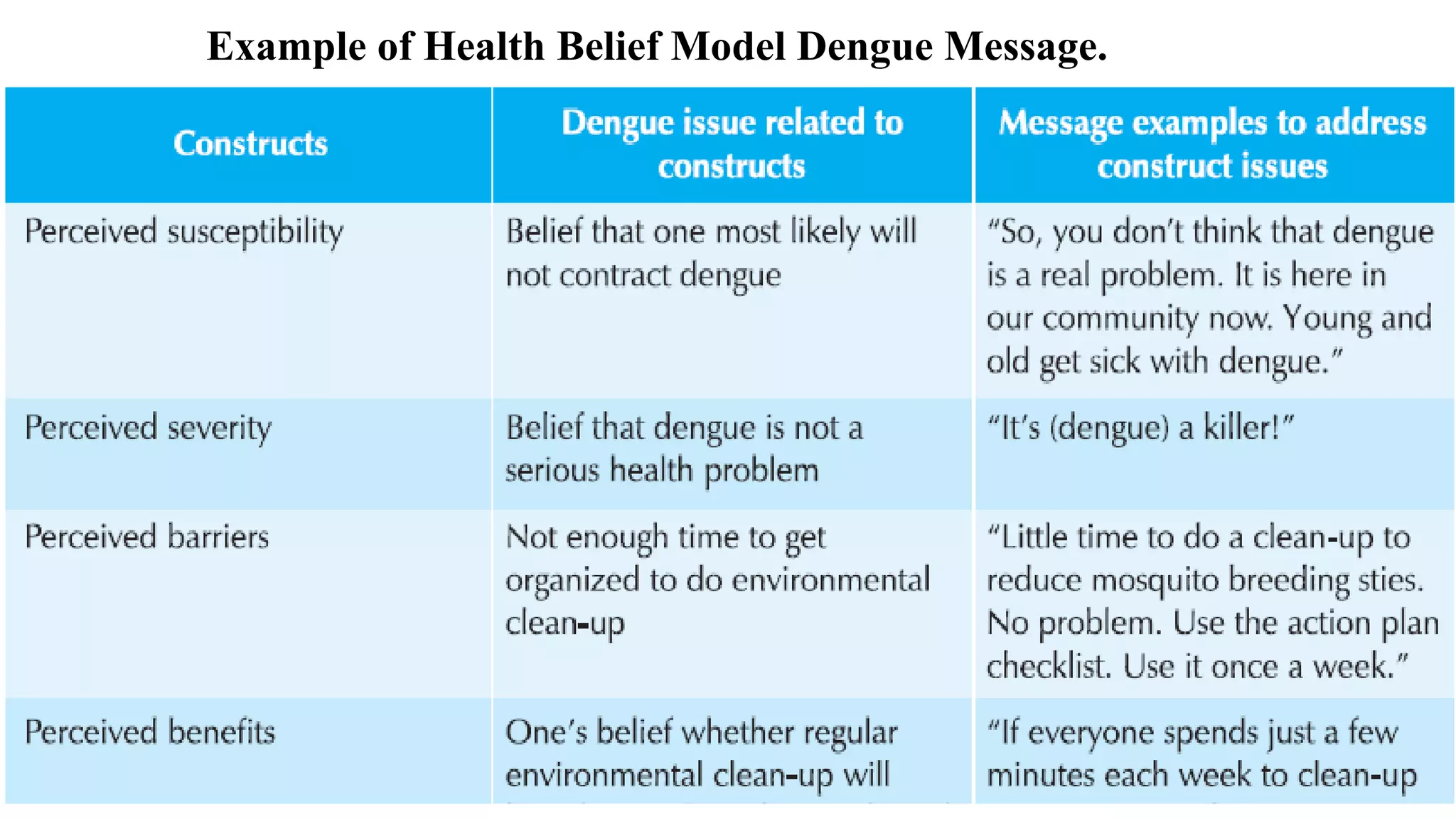
The Health Belief Model (HBM) is a theoretical framework used to understand health behaviors. It was developed in the 1950s to explain why people failed to adopt disease prevention strategies. The HBM suggests that a person's health behavior is determined by their perceived susceptibility, severity, benefits, and barriers of a health problem and the cues to action that trigger decisions. It includes six constructs: perceived susceptibility, severity, benefits, barriers, cues to action, and self-efficacy. The HBM is widely used but has limitations such as not accounting for attitudes, habits, or environmental factors that influence health behaviors.