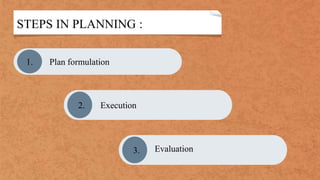
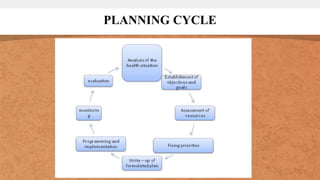
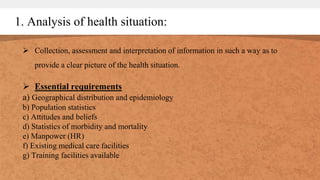
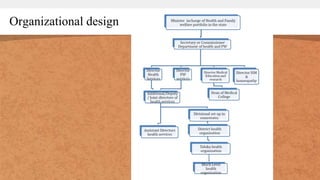
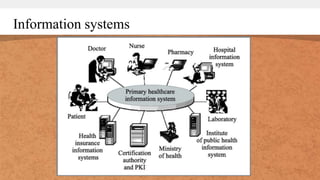
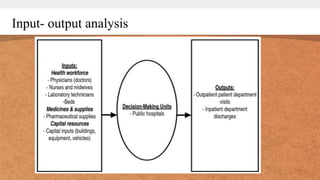
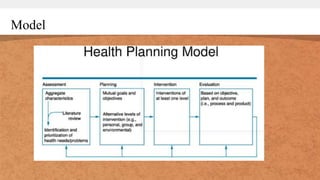
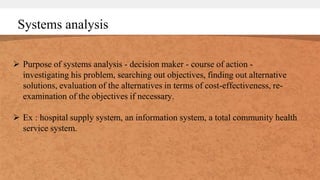
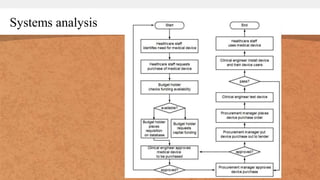
This document discusses health planning and management. It defines health planning as the orderly process of defining health problems, identifying unmet needs, establishing goals, and outlining plans to accomplish objectives. The planning cycle involves analyzing the health situation, establishing objectives and goals, assessing resources, prioritizing issues, developing plans, programming and implementing plans, monitoring progress, and evaluating outcomes. Health management methods discussed include organizational design, communication, information systems, and quantitative methods like cost-benefit analysis and systems analysis. The key steps in health planning and tools for health management are outlined.