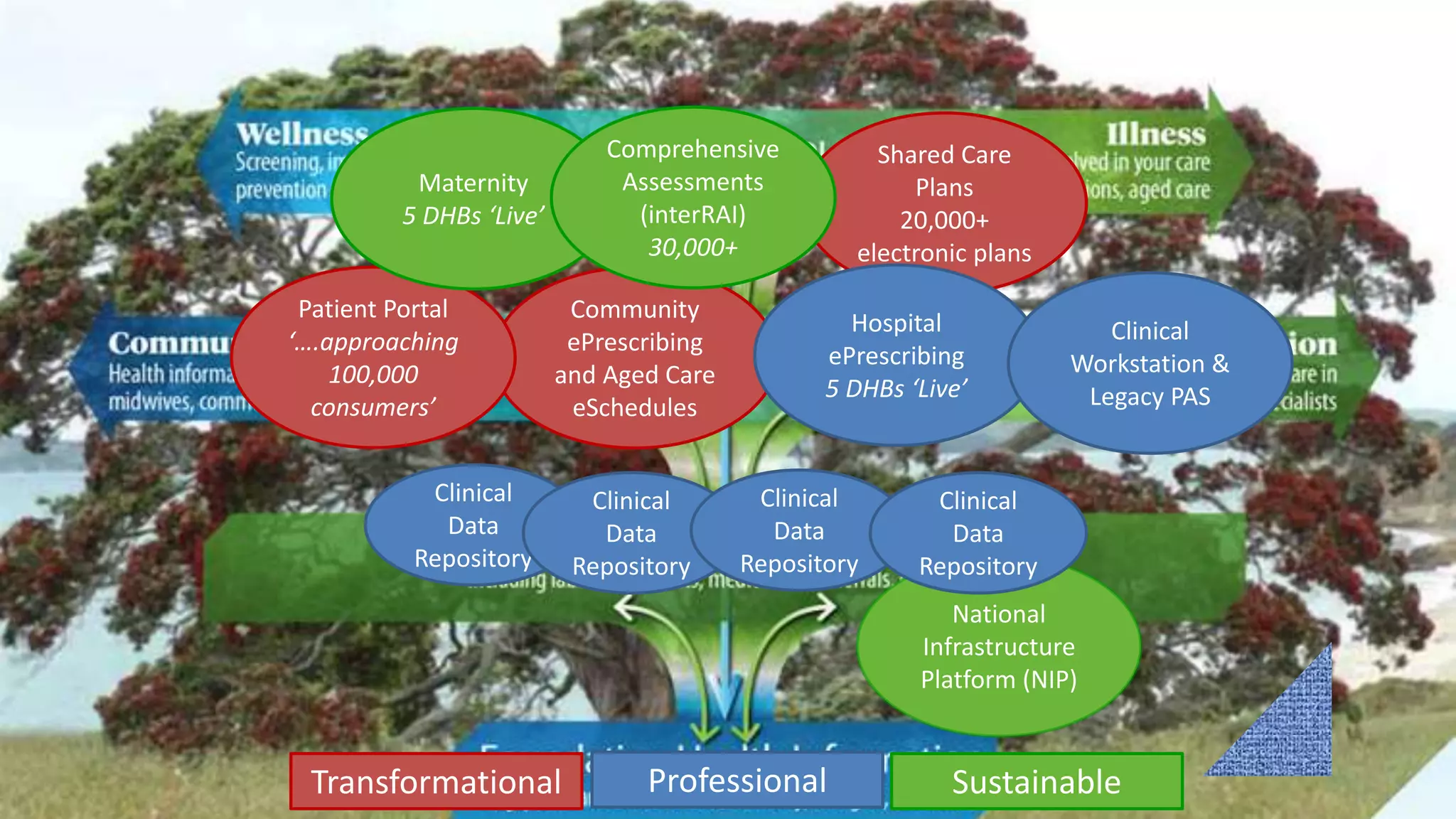
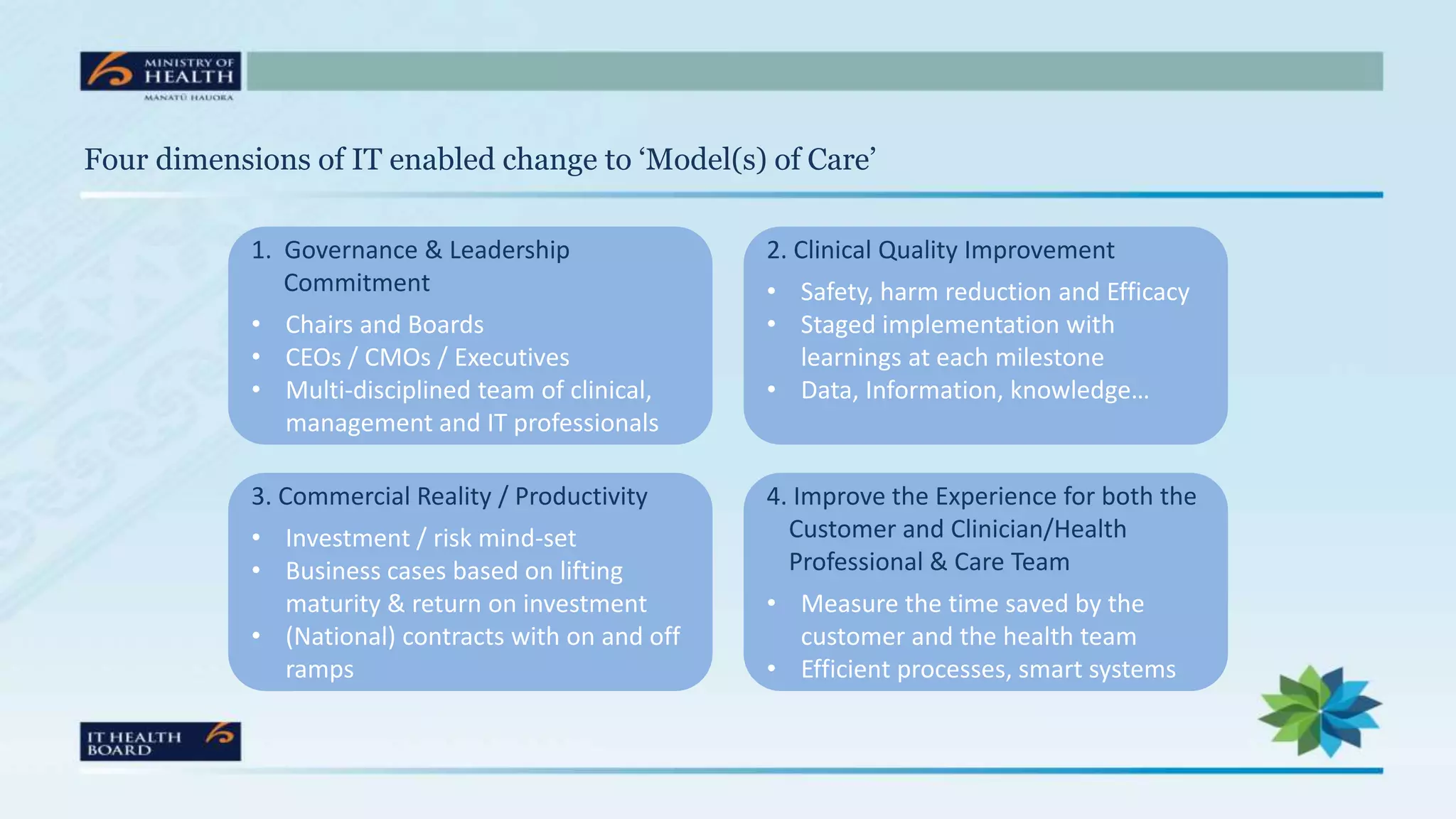
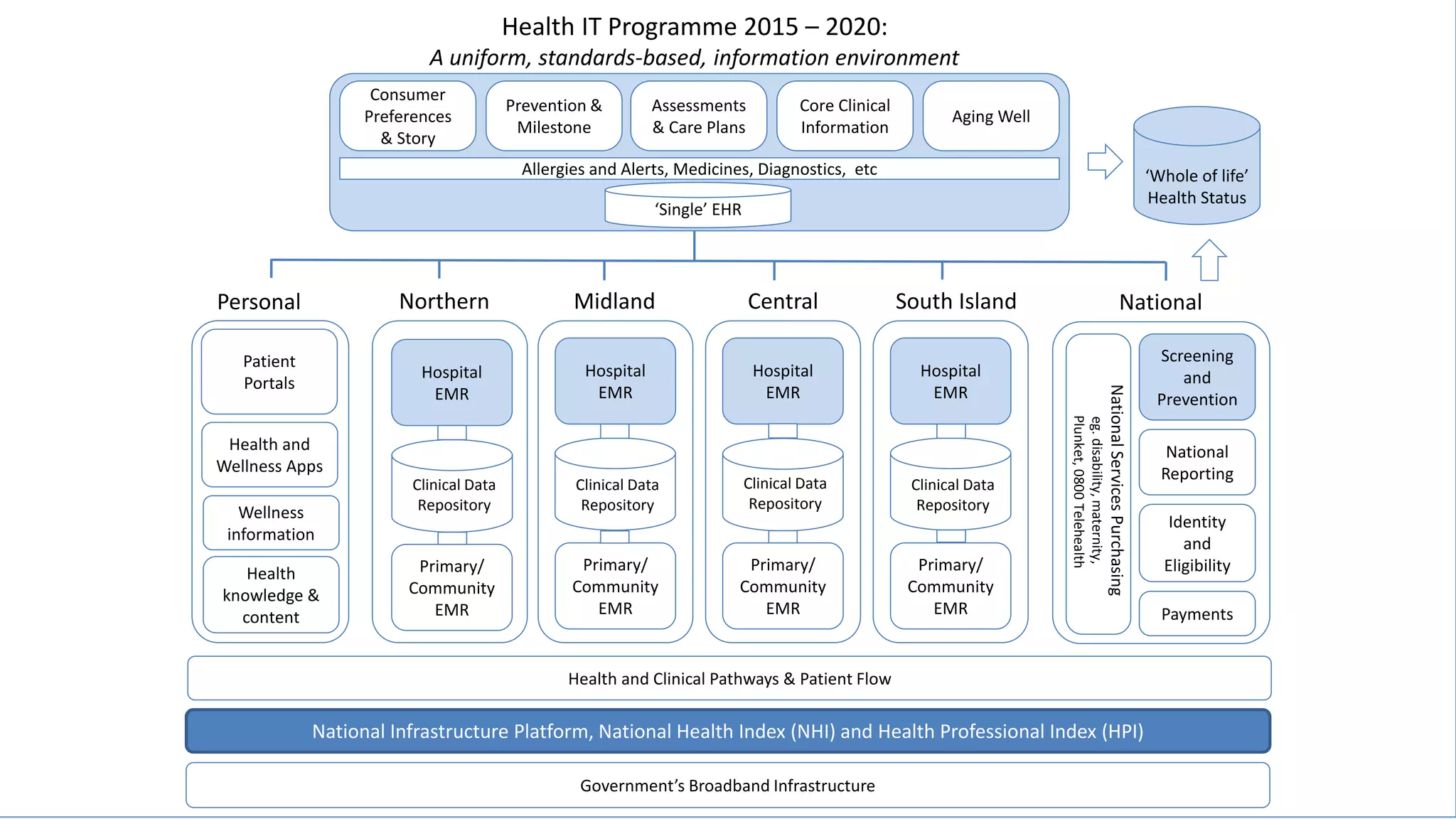
The document discusses New Zealand's Health IT Programme from 2015-2020. The program aims to create a uniform, standards-based health information environment for New Zealanders. It focuses on 4 key areas: 1) establishing a single longitudinal electronic health record, 2) creating a common digital hospital blueprint, 3) designing an IT prevention platform, and 4) using data to support health and social investments. The next steps are to design implementation plans over the next 6-9 months and benchmark hospital EMR maturity in 2016. The goals are to improve the customer and clinician experience, support prevention, and increase efficiency and productivity across the health sector.