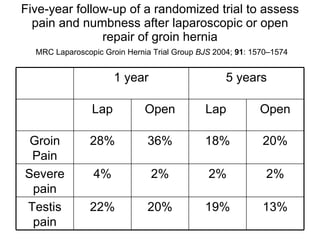
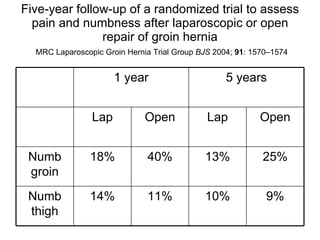
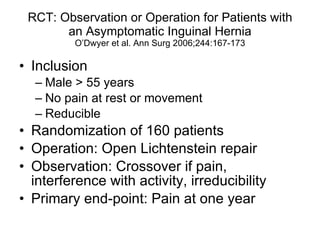
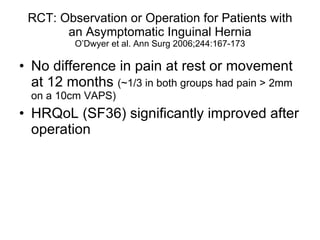
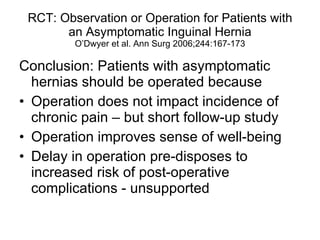
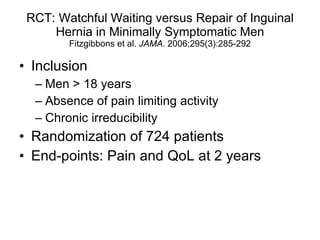
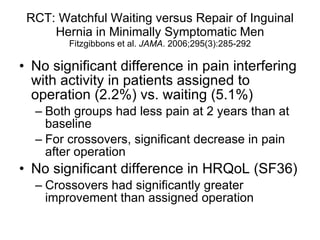
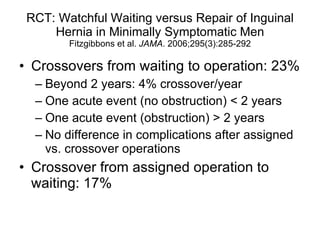
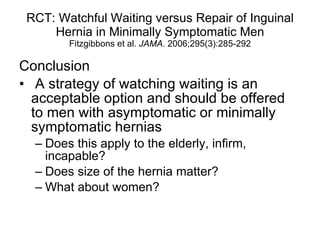
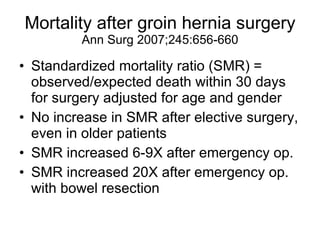
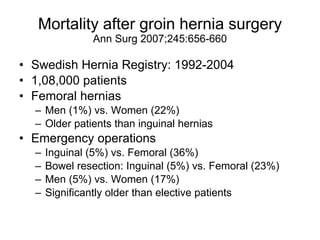
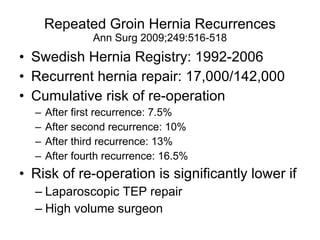
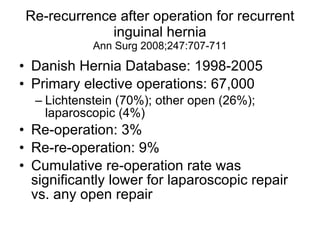
While some studies have found no difference in chronic pain outcomes between early hernia repair and watchful waiting for asymptomatic hernias, watchful waiting remains a reasonable option to offer patients. Emergency hernia repairs and repairs involving bowel resection have significantly higher mortality rates than elective repairs. Recurrence rates are higher with each additional hernia repair, though laparoscopic TEP repair and repair by high volume surgeons may lower reoperation risks compared to open repair.