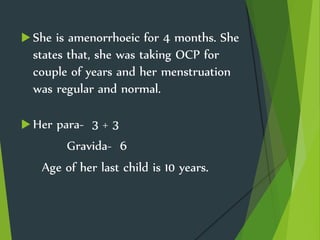
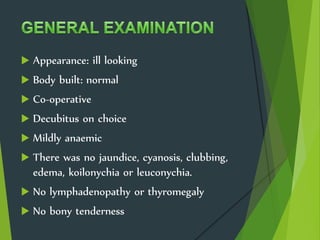
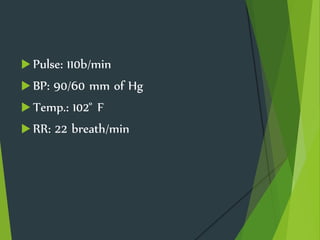
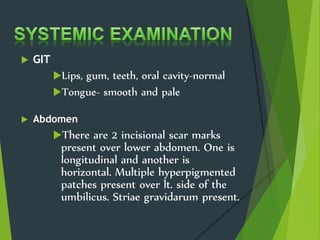
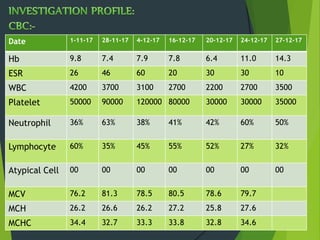
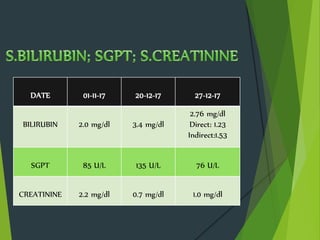
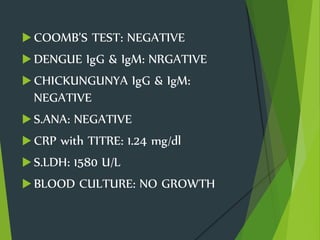
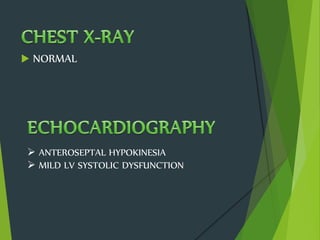
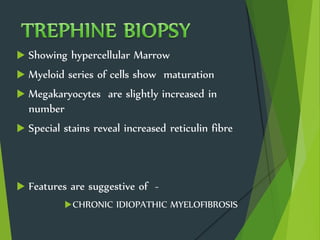
A 42-year-old diabetic woman presented with 2 months of high fever. She had been previously admitted twice for the same symptoms and diagnosed with a urinary tract infection and suspected myelodysplastic syndrome. On current admission, she displayed pancytopenia. Bone marrow biopsy revealed features suggestive of chronic idiopathic myelofibrosis. Her fever, pancytopenia, hepatosplenomegaly, and bone marrow findings indicate a diagnosis of chronic idiopathic myelofibrosis exacerbating her diabetes.